By the time Steven Mitchell made it—by foot—to the Churches Joint Council on Human Needs food pantry in Benton, Arkansas, on a cold November day, his two hernias had him limping in pain. A few weeks before, he had received a letter from the state’s Department of Human Services informing him that his Medicaid health coverage had been cut off. This was the first that Mitchell had heard of the state’s new work requirement for Medicaid recipients, which as of June 2018 required many enrollees to spend 80 hours each month working, in school, or volunteering and to log those hours online in order to maintain their health benefits. Getting that letter “messed me up a lot,” Mitchell said, in a gravelly voice deeper than his young face would indicate. Before the state’s Medicaid program was expanded in 2014 to cover low-income adults without children, Mitchell didn’t have any insurance. He never had annual checkups; Medicaid has meant getting diagnoses he didn’t know about. “I knew I had a hard time with my breathing,” he said, “I just never knew I had asthma.” After Medicaid’s expansion, Mitchell got access to an inhaler and a breathing machine as well as pain medications for his hernias and other ailments. “It was a relief,” he said. “I got to get on top of a lot of things, and [it] helped me get a little better.”
Now he’s back to square one. Without insurance, Mitchell hasn’t been able to get any of his medications. He had an appointment with his surgeon to deal with the hernias just two days after I met him, and he wasn’t sure whether the doctor would see him.
But for Mitchell, working is far easier said than done. He’s struggled with hernias and asthma all his life. Each time he tries to work, he either winds up in the hospital or has to quit due to the pain and frequent doctor appointments. “I always end up paying for it in the end,” he said. “That’s the real thing that stops me from actually getting out to work.”
Mitchell has had a case pending to get on disability insurance for what he estimates has been two years. If he were to be approved, he would get monthly disability benefits in addition to being automatically exempt from the work requirement. But in early November, a decision still hadn’t come through. (On average, applicants for disability in Little Rock wait over a year to get a hearing.)
Outside the food pantry, as Mitchell prepared to set off on foot again in search of help with his utilities, he said he didn’t see the point of the work requirement. “No one should be forced to work if they’re not able to,” he told me. Health insurance “is just something that people need. The medication and getting these treatments is what will help us get back to work if we’re able to. Not having insurance, you can’t do any of that.”
In 2017, the Trump administration announced that, for the first time in history, the Centers for Medicare and Medicaid Services would approve state requests to impose a work requirement on the low-income people who rely on Medicaid for health insurance. Arkansas was the first state to implement one. Starting in June, everyone age 30 to 49 who had enrolled in the state’s Medicaid expansion became subject to it, which meant that unless the state determines that they’re exempt—because they already have a job, a disability, or young children at home to care for—they must log on to a website every month to report their compliance in order to keep their coverage. If they fail to do so for three months in a row, the Department of Human Services cuts off their Medicaid coverage.
Popular
"swipe left below to view more authors"Swipe →A number of other states, including Arizona, Indiana, Kentucky, Michigan, New Hampshire, and Wisconsin, are chomping at the bit to follow suit. Arkansas offers the first glimpse at the impact that a work requirement will have. The policy has only been in effect for nine months, but the results are clear: Arkansans are being thrown off of Medicaid in huge numbers. Meanwhile, unemployment in the state has hardly budged.
Since June, a total of 18,164 people in Arkansas have lost their Medicaid coverage because they failed to comply with the work requirement. It’s a staggering number, advocates say, given that the state had estimated some 38,000 people would fall under it. “I certainly expected people to lose coverage,” said Joan Alker, executive director of the Center for Children and Families at Georgetown University. “It is fulfilling my lowest expectations.”
Losing health insurance often triggers a cascading set of crises for former Medicaid recipients. In Tennessee, when 170,000 people lost coverage in 2005, residents received less medical care and saw their health worsen. The positive effects of expanding Medicaid, on the other hand, are wide-ranging and well-documented. Nationally, expansion has meant greater access to and use of medical care, improved health, and fewer deaths. It has also been found to reduce unpaid bills and medical debt and keep people out of bankruptcy.
Eight years ago, Donald Underwood was hit by a stray bullet. He lost his right eye and suffered serious brain damage. Since then, Underwood, a bright, balding man, has been hospitalized 27 times for schizophrenia, major depressive disorder, psychotic episodes, and seizures. He takes a cocktail of medications, including barbiturates, heart medications for arrhythmia, seizure medicines, a beta blocker, and an antiretroviral for HIV. They cost $12,000 a month; Medicaid pays for six of them. “Because of my medications and what I’ve been able to get through Medicaid,” Underwood told me, “two months ago, after nine years, I won my first game of chess.”
But now he’s subject to the work requirement, and in November was set to lose his coverage in two months. Underwood had no idea where he could possibly find work. He’s considered legally blind and has frequent seizures caused by his sensitivity to flashing lights, auditory input, and stress, making him an unlikely hire: “So I get a job, right? I hope they don’t have LED lights. I hope they’re not playing loud music in the background.” Like Mitchell and many of the other people I spoke with, Underwood has a case pending to get on disability insurance, but hasn’t been accepted yet.
“Every time my heart skips, I think about when I can’t get the medicine next month,” he said. He gives himself six months to live if he’s cut off from his medications. “I count on my health insurance to keep me living.”
The state defends the requirement by saying that with unemployment so low—3.7 percent in Arkansas as of December 2018—people who can work should have to in order to receive benefits. Those who don’t comply “don’t value the insurance,” Cindy Gillespie, director of the Arkansas Department of Human Services, suggested. But if the work requirement were functioning as promised, significant numbers of Arkansans would be reporting that they went to work for the first time after it was implemented. In January, just 322 people logged onto the website and reported work activities. And even among those, it’s impossible to know how many are newly employed or were already working, possibly under the table or for fluctuating hours that wouldn’t have shown up in state databases.
Jennifer Daniels would seem to be a success story. She got a letter from the Department of Human Services telling her that she would have to report work activities to keep her Medicaid coverage, so she went online to comply. There, she discovered that the requirement was as much about paperwork as about an actual job. The process was “frustrating,” she said. “They take you one step, then you had to do two or three more.” She doesn’t have a computer at home, so she did it on her phone, which took her about an hour and a half—a process she has to go through again each month.
Daniels has a paying job, but that was true long before the work requirement. The 42-year-old, decked out in a matching University of Arkansas Razorbacks hat and hoodie, has been working as a certified nursing assistant since she was 16, usually full time. Today, she works at a nursing home, a job she loves and held four months before the work requirement even went into effect. “There’s nothing wrong with working,” she said, but the reporting process is “too much.”
The work requirement is based on harmful stereotypes of the poor, advocates say. It “assumes people are completely disengaged and disconnected from their community, which just isn’t true,” said Marquita Little Numan, president of the Urban League of the State of Arkansas. Nationally, Medicaid recipients are very likely to work, and those who don’t usually have a disability or other reason they can’t. Kevin De Liban, a staff attorney at Legal Aid of Arkansas, calls work requirements “termination traps.” They are, he said, based on twin myths: that the poor are lazy, and that the requirement will get them to work. “Work requirements do not address any actual problems faced by our clients,” he added.
Before the imposition of the work requirement, Arkansas was making major strides in reducing the number of uninsured residents in the state. The number of uninsured children had dropped from 7 percent in 2013 to 5 percent in 2017, and the rate of uninsured adults was falling too, from 24 percent in 2013 to 12 percent in 2017. Since the Medicaid expansion, advocates have been working hard to help people learn how to access care, particularly preventative services. But now that progress is being undermined. “Without coverage, folks are just going to revert back to that old way of doing things,” Numan said. “I think they’ll just avoid it.” Mental-health providers face a particularly uphill battle. “Even on our best effort on our best day, keeping clients engaged in treatment is always a challenge,” said Kathy Harris, CEO of the Southeast Arkansas Behavioral Health System community mental-health clinic in Pine Bluff. Losing insurance makes it even less likely that people will come in for therapy sessions or take their medications. “They go without coverage, they go without health care, they don’t see a doctor, they don’t have medications,” said Kymara Seals, policy director at the Arkansas Public Policy Panel. “We’ve known people that died.”
Even for those able to comply with the work requirement, there are plenty of barriers to finding steady work in the state. In Clarendon, Mary Kersey, an enrollment specialist at the Mid-Delta Health Systems clinic, noted that the biggest one is the dearth of jobs. Most people who are employed work on farms; others might be able to get a job at the town’s sawmill or at the Belleville shoe factory in DeWitt, about an hour away.
According to Danny Stanley, CEO of the Southwest Arkansas Counseling and Mental Health Center, this is what he hears from the people he serves in Texarkana: “There are no jobs in southern Lafayette County. There’s no place to volunteer. And I don’t have transportation even if I did have a job.” Pine Bluff has a paper-products plant, a Tyson chicken plant, and a transformer manufacturer, but not much else. Assuming that a Medicaid recipient did find a job, it’s unlikely to offer health insurance, even though moving people from Medicaid to employer-based insurance is one of the stated goals of the work requirement. And even if it did, the Urban Institute found that the insurance would cost the average Arkansas minimum-wage worker more than 8 percent of her income.
There are even fewer job possibilities for a Medicaid recipient with severe mental illness. Those in treatment have to take time off from work regularly to go to their appointments—something a low-wage employer might not tolerate. “You can’t just do it like a broken arm, and it’s healed and life goes back to normal,” Harris said. “These are illnesses that are not going to go away.”
The state has been adamant that it won’t spend any additional funds to help Medicaid enrollees find work. There are existing supports for those who have to meet work requirements for food stamps, and some people are being referred to job-search and job-training assistance at the state’s Department of Workforce Services. But neither program has room to handle everyone who would be eligible. “There are no efforts here to support work,” Alker said. “No new resources for job training or child care or the kinds of things that would reduce barriers.”
This, advocates say, is evidence that the motivation behind the work requirement was not about jobs, but rather thinning Medicaid’s rolls. It wouldn’t be the first time that Arkansas has tried to do so. In its proposal to the Centers for Medicare and Medicaid Services, the state also asked to reduce the eligibility threshold for people to enroll in Medicaid. (That request was denied.) In 2017, the state began requiring recipients to report any change of address and to respond to letters requesting verification of their addresses within 10 days or lose coverage, leading to around 26,000 people losing their Medicaid benefits.
In fact, Arkansas’s work-requirement policy is the latest stage in a decades-long project on both the state and federal level to make it harder for poor people to access safety-net programs—an effort that has taken on a new intensity under the Trump administration. In the 1990s, President Bill Clinton championed work requirements for cash assistance, which were made more draconian by congressional Republicans like Newt Gingrich. Welfare, now known as Temporary Assistance to Needy Families (TANF), is the only public program with blanket work requirements, but Republicans have been trying to impose them on other programs ever since. Former House Speaker Paul Ryan called the 1990s reform an “unprecedented success” when defending his own budgets’ massive cuts to safety-net programs. Ryan left Congress last year, but Trump’s administration has taken up his mission. In July, the Council of Economic Advisers released a report making the case for imposing work requirements on everything from Medicaid to food stamps to housing assistance. In an executive order last April directing federal agencies to look into imposing work requirements on their own programs, Trump asserted that these requirements “reserv[e] public assistance programs for those who are truly in need.” His 2018 budget called for encouraging work in “welfare programs” so that able-bodied adults who don’t work won’t “take…away scarce resources from those in real need.”
Despite such rhetoric, work requirements—to put it simply—do not work. Research has consistently found that poor health, including untreated mental illness, makes people more likely to lose their jobs, while health insurance helps them get and keep work. Medicaid-expansion enrollees in Ohio, Michigan, and Montana were better able to work once they had coverage; losing one’s Medicaid, on the other hand, doesn’t lead to any gains in employment. The same is true for TANF: The work requirement hasn’t resulted in increased employment, but rather in increased poverty.
Arkansas has told advocates that people who lose health insurance can avail themselves of free care at community health and mental-health centers. But after Medicaid expansion, the system was changed to account for the fact that people finally had health insurance to cover the cost of their care. As a result, many community health centers no longer have uncompensated-care funds to cover people without insurance. If they once again have to provide such care, they may have to cut services—or close their doors. And community health centers are no replacement for health insurance. They don’t fully cover the cost of prescription drugs, nor do they offer specialist care. “Referring out becomes the issue,” Kersey said. If her patients need an MRI, for example, they can’t get it done at her center, which means they’ll likely be on the hook for hundreds of dollars to pay for it.
Then there’s the fact that the Medicaid expansion has kept Arkansas’s rural hospitals from closing. Since 2010, the state hasn’t seen a single rural hospital close—unlike every one of its neighbors that didn’t expand Medicaid. Now, the stability of those hospitals is at risk.
Like Steven Mitchell, Kristie Cameron learned that she was subject to the work requirement the day she found out she was losing her Medicaid coverage. If the Department of Human Services sent her a letter informing her of the requirement before that, she wouldn’t have received it: As a victim of domestic violence for the past 20 years, whose abuser frequently follows her wherever she tries to set up a home, Cameron moves constantly. The only reason she received the DHS letter telling her she was cut off was because some mail had been forwarded to her mother’s house.
The frail-looking 45-year-old, with piercing blue eyes and stringy blond hair, standing in the Beebe Christian Outreach Center food pantry in boots far too large for her, doesn’t have paid employment. She has a car, but it’s not registered and she doesn’t have a driver’s license; that makes getting to jobs difficult. She also doesn’t have access to the Internet to report compliance unless she goes to her mother’s house in Garner, one town over from where she’s staying now. She has a phone, but it recently got cut off. While she doesn’t work formally, she does odd jobs to give back to her community: She helps an elderly woman do physical therapy and looks after her dog. She cares for stray animals all over town.
Cameron sees a doctor regularly for her insomnia and deals with frequent blood-sugar lows. She has vision problems in one eye. But without Medicaid, “I’m going to wing it,” she said, “take care of myself like I always have.”
Many of those targeted by the work requirement are as difficult to reach as Cameron. They may be chronically homeless, or living with significant mental illness, or forced to move frequently. They may not have the money to add minutes to their phones; their numbers may change often. Staffers at the Pine Bluff center made a list of clients they thought might be subject to the work requirement and started to call them. “A huge number of those we weren’t even able to contact,” Harris said. “The ones we were able to contact had no idea or understanding of this reporting requirement.” Danny Stanley hears the same thing from his clients: “‘I don’t have Internet access. I get this letter in the mail, I don’t really know what it means.’ So they put it aside or throw it away.”
“We’re taking for granted that people receive their mail on a daily basis like middle-class Americans, and that’s just not true,” said Mandy Davis, director of the resource center Jericho Way. Homeless residents, for example, may have their mail sent to day centers but don’t necessarily pick it up every day. “I’ve got a stack of DHS letters in there for people I haven’t seen in months,” said the Rev. Paul Atkins, who runs the Canvas Community Church. “Sometimes I can get a hold of them, but [some] are not findable. Sometimes they don’t want to be found.”
Reaching this population would take serious resources and time, but the state devoted no additional funding to outreach. Even those who received DHS letters didn’t necessarily understand them. “I have a lot of people that just come in with their letters [and ask], ‘Tell me what this means,’” Kersey said. Across the state, 14 percent of the population lacks basic literacy skills.
Even if a Medicaid recipient manages to find a job, reporting work hours or logging an exemption is mind-bogglingly complex. First, a recipient must have received the DHS letter, which includes a personal-identification number, or PIN. (Some of De Liban’s clients have reported being sent PINs that don’t work; others who never received the letter don’t have a PIN to begin with.) That PIN has to be linked to their health-care account—and that requires an e-mail address, something that many people don’t have. Until December 19 of last year, compliance could only be reported online—to save money, the state explained. (There is now a phone-reporting option.) That presented a huge problem, given that 18 percent of the population has no access to the Internet. (Arkansas has the second-lowest rate of home Internet access in the nation.) In Clarendon, most of the people who come to the Mid-Delta Health System don’t have a computer at home; there is one public library where people can use the Internet. Also, getting to the page to report compliance requires clicking through three other pages first—and the online portal shuts down every day between 9 pm and 7 am.
Those who are trying to comply but struggle to do so have few places to turn. At the Department of Health Services office in Pine Bluff, a video about the work requirement played to a mostly empty waiting room. Narrated by a white woman in a red coat, the video claimed that “there are plenty of people willing to help if you reach out.” But it directed people to call the nonprofit Arkansas Foundation for Medical Care. No additional DHS staff were hired to help people navigate the system.
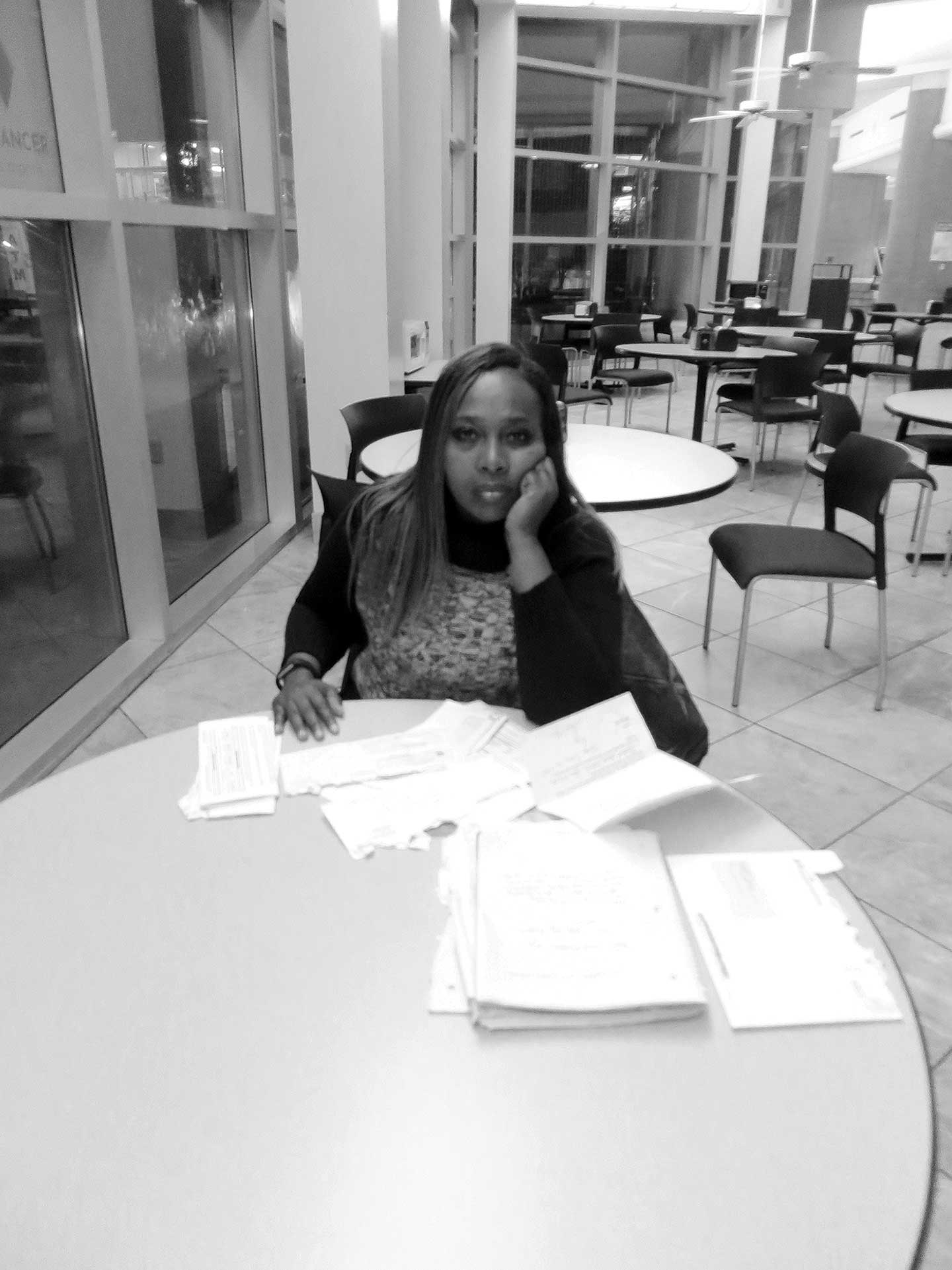
LaJoy Person is impeccably organized. When she arrived to our interview in November— her long eyelashes perfectly done, her honey hair the same color as her skin—she plopped down a stack of paperwork: bills, letters, receipts. “I’ve never dropped the ball on nothing that I need to turn in for my kids,” she said. “Never.” So when she got the letter about the work requirement, she went to a DHS office to find out exactly what she needed to do. She was told that because her son was under 18, they were both exempt, and that when he turned 18, she would get another letter telling her what she needed to do to keep their coverage. Eleven days after her son’s 18th birthday on September 19 of last year, she received a letter saying they were both cut off. But the medical bills didn’t go away. After their coverage ended, her son, who plays football and basketball, received a bill for treatment of an inflamed knee; Person kept a physical-therapy appointment for her own neck and back pain—if she didn’t, it would have been hard to get another—and that cost her $200. She paid over $100 out of pocket for her pain medication. To cover those costs, she borrowed money. She feared that her stress would increase her blood pressure, which was already high. She was most worried about her son losing coverage, though that appeared to be a mistake: He should still qualify for ARKids, a state Medicaid program for children, because he’s under 19. “It makes me feel like I’m not good enough of a parent because I don’t have health care for my child,” she told me.
Person spent hours on the phone calling various numbers to find out how to get their coverage back. She was repeatedly transferred among representatives and departments. She once got transferred to a supervisor whose voice mail was full. Then she was transferred to another voice mail, and another. No one she spoke with knew the status of her case.
It wasn’t until early December that she finally got their coverage restored. “It seemed like forever; it was a struggle and very stressful,” she said. She finally decided to go to a DHS office and refuse to leave, staying after hours with a supervisor until the matter was resolved. Eventually, the DHS staffer “said to me, ‘Mrs. Person, today you and your son’s health care has been reinstated.’ I cried right there on the spot like a baby!” she said. “That day, I got my sigh of relief—I got my peace back.”
Person still gets letters from the Department of Human Services about the work requirement that she finds “very confusing,” but she’s doing everything she can to stay on top of the paperwork so that she and her son don’t get cut off again.
As of November, Jolene Seale had been clean for two and a half months; she should qualify for a work-requirement exemption for going into drug rehab, and reported that in August. But she didn’t have access to a phone in either September or October, while she was at the facility. During those months, “I didn’t even think about [reporting my status for] my work requirement,” she said.
She didn’t know she had lost her health insurance until after she left treatment; she went to pick up her prescription refills at a Kroger and was told that her insurance had been denied. “I cried,” Seale recalled. “I said, ‘Oh my God, what am I going to do now?’” She should be taking arthritis medication, a drug for her restless-leg syndrome, medication to combat a recently contracted STD, and psychiatric drugs, all of which were previously covered by Medicaid. The night before we spoke, she couldn’t fall sleep until 4 am because she hadn’t taken the medication she needs. “I want to stay on my meds, because I’m trying to stay clean,” she told me. The lack of sleep can make her feel like she may as well get high instead. “I don’t want to do that… I need my insurance.”
Many Arkansans found out about the work requirement the same way Seale did: They went to the pharmacy or doctor and were told they no longer had health insurance. At that point, it was likely too late for them to do anything about it: After three months of noncompliance, Arkansas’s policy locks people out for the rest of the calendar year, so those who lost coverage last year didn’t get a chance to reenroll until January. “There’s really no reason for that,” said the Center for Children and Families’ Joan Alker. “It’s essentially forcing people to be uninsured for a period of time as a punishment.” As of December, fewer than 1,000 people had reenrolled.
That lockout period gets more punitive this year. People who lost coverage last September were able, in theory, to regain it four months later; those who lose it in early 2019 will go without coverage for the rest of the year. The pool of people subject to the requirement has also expanded: Though 19- to 29-year-olds were exempt last year, now they have to report.
There are some things that Arkansas has gotten right, experts say. By reviewing its data on who has a young child at home, who is already meeting the work requirement in SNAP, and whose reported income indicates they work at least 80 hours a month, in November the state automatically exempted 53,975 of the 66,628 people subject to the requirement.
A catch-all “good-cause exemption” could spare even more people. The homeless, for example, are not automatically exempt from the work requirement, but the state has indicated that they could get excused that way. Other potential good-cause exemptions that the state has enumerated include domestic violence, a birth or death in the family, natural disasters, divorce, and “other.” But the exemption, which was added at the last minute, is one of the most confusing parts of the policy. Advocates aren’t sure who makes the final decision about it. Between June and January, the state reviewed 904 requests and granted just 633.
When he got his notification letter from the DHS, John Rullmann didn’t read the whole thing. He is “one of the local homeless,” as he puts it, living in a forest by the edge of a river. His mail gets sent to the Vine and Village Church in an old gym in a strip mall. While he knows all of the places that offer free Wi-Fi—the church, McDonald’s, Taco Bell, a car dealership—he doesn’t have a phone to get on the Internet. As someone without a home, Rullmann could potentially request and receive a good-cause exemption. But that would require him knowing about the work requirement and figuring out how to ask for an exemption.
In order for the Medicaid expansion to continue, Arkansas’s legislature has to re-fund it every year. And state lawmakers have made it clear that the imposition of a work requirement is the price of Medicaid expansion. That puts advocates in a tricky place. De Liban argues that no matter how well or poorly work requirements are implemented, when applied to Medicaid, they’re simply illegal. Along with the National Health Law Program and the Southern Poverty Law Center, he represents nine plaintiffs who are suing the state, the federal Department of Health and Human Services, and the Centers for Medicare and Medicaid Services over the policy. Medicaid is “a medical program for health insurance,” De Liban pointed out. “Health and Human Services doesn’t have the authority to just, on its own, impose work requirements on a health-insurance program when there’s no basis for it anywhere in the law.” That differs from the laws governing TANF or SNAP food stamps, which do allow for the imposition of work requirements.
Would the lawsuit, if successful, put Medicaid expansion at risk? “The fact is that work requirements are clearly illegal,” De Liban said. “There are plenty of reasons to be able to justify continuing Medicaid expansion just based on its own merits.” But the Arkansas legislature may not agree. “I think it would be unrealistic to think that it will be easy to keep an expansion program if this goes away,” Numan said.
Since January 2018, 14 other states have requested the ability to impose their own work requirements on Medicaid. They would be wise to take stock of what’s happened in Arkansas. “Don’t do it,” said Numan, adding: “There’s no good way of implementing this kind of policy.” Even federal agencies are taking note. In November, the Medicaid and CHIP Payment and Access Commission, a nonpartisan legislative-branch agency, sent a letter to Health and Human Services Secretary Alex Azar calling for the department to hold off on approving work-requirement requests based on the situation in Arkansas. In February, Senator Ron Wyden (D-OR) and Representative Frank Pallone (D-NJ) also wrote to Azar urging him to stop approving Medicaid work requirements, saying their concerns have “play[ed] out in real life in the State of Arkansas.”
Numan wishes the state had put its energy into helping people get the support they need to work, such as education, child care, transportation, and, of course, health care. The very idea of work requirements in Medicaid makes little sense. “Medicaid is a work support,” Alker asserted. “If you want to support work, it makes sense to expand Medicaid. If you want to stigmatize the program and [add] a lot of red-tape barriers, then do a work requirement.”