The Search for Special Case–Baby 1
Who was buried in the lonely grave in New York’s potter’s field? The year-long search led to a lost world in the history of AIDS.

This story begins, for me, on an island—a small island that sits at the northeastern corner of New York City, in a shallow basin at the edge of Long Island Sound. It’s a lonely place, exposed and windswept, its shores eaten away by the currents. On maps, it looks like little more than a squiggle, a scratch left by a careless cartographer. If you didn’t know to look for it, you wouldn’t see it.
Like many New Yorkers, I didn’t know to look for it for most of my life. I had no idea this place, Hart Island, existed or that, for much of its recent existence, it has served as an offshore repository for those deemed alien or undesirable by the guardians of city life. Prisoners of war, victims of yellow fever, miscreant boys, sickly consumptives—all did time in the red brick buildings that once dotted the island. Mostly, though, for more than a century and into the present, the island has served as the final resting place for scores upon scores of the city’s dead.
Hart Island is New York City’s public cemetery, its potter’s field, where the unclaimed, unidentified, and indigent are buried. As many as a million people have been laid to rest here since 1869, both adults and children, and among them are the victims of almost every plague that has struck the city—from tuberculosis and typhus to AIDS and Covid—along with the more enduring afflictions of poverty and aloneness. Some people have chosen to be buried there—because it is free, because it is communal—but many have not. Instead, they more or less drifted there, pulled by the currents of addiction, mental illness, stigma, or neglect. From the margins they came, and to the margin they were sent.
To visit this place, as a living person, is a somewhat more complicated proposition. Much like another well-known netherworld, Hart Island can be reached only by ferry and is off-limits to most of the public. Even so, stories have made their way from its shores over the decades—legends and myths, shards and fragments, fables, yarns, and a few gemlike oddities. These include the usual paranormal fare—accounts of silhouettes in the fog and the like—but the majority, and by far the most interesting, are the tales bound in fact: the ones of real people, stacked three high in mass trenches, whose lives read like an alternate history of New York City.
Among the most curious of these is the story of a child. This child lies in a grave that is different from most of the others: It is half-hidden at the southern tip of the island and is separated not only by distance but by the fact that it contains just a single body. On the grave’s marker, there is a runic sort of inscription that reads “SC-B1 1985.” If you Google about for an explanation, you will find—via both official New York City websites and various news sources—that it stands for “Special Child–Baby 1” and the year of their burial, 1985. You will also find this: The grave belongs to the first child to have died of AIDS in New York City.
This, however, is all that you will find. The child’s name and age, the date of their death, the reason for their interment on Hart Island—none of that is known. Nor will you find any of the hazier details that make up a life, like the color of the child’s eyes or the sound of their laugh or the timbre of their cries. There is only the one assertion—this was the first child to have died of AIDS in New York City—and the nothingness that surrounds it. A mystery.

In late 2022, I joined a dream team of journalists from WNYC, including my former Nation colleague Kai Wright, to work on a podcast about the early days of HIV and AIDS in New York City. Our mission was to chart the stories of the many people who were shoved to the sidelines of the epidemic—poor people, Black and brown people, women, injection drug users—but who refused to stay out of sight. We decided to call the podcast Blindspot: The Plague in the Shadows.
Among the quests I set myself was to try to unearth the story of SC-B1. I had learned about this child in 2009—not long after I stumbled upon the existence of Hart Island and went on a days-long Google bender to find out as much as I could about the place. Until then, I had never heard of any child who had died of AIDS and been buried there. I had never even heard of a child dying of AIDS in New York City. I remembered Ryan White, of course, the brave teenager who was barred from attending his Indiana middle school for having HIV and later died, in 1990. But I could conjure up nothing from my own childhood in 1980s New York about a kid who had died of AIDS and then been transported to this isolated island-place. This fact ate at me.
So I became curious—obsessed, even—thinking about the child, wondering who they were. Years later, when I finally began reporting, my hope was that I would be able to uncover SC-B1’s identity and be able to tell their story—to explain how such a tiny person had come to have AIDS and why they had wound up on Hart Island, and who their parents were and what fate had befallen them. I came to suspect, particularly as I did more research, that this story might reveal something essential—about the early days of AIDS, yes, but also about New York City, and about the intimate, intertwined relationship between the two.
During the months I spent reporting, I interviewed dozens and dozens of people, revisiting a past that still has the power to pummel and cause pain. I spoke to doctors and nurses who had looked after children on pediatric wards—heroic types who’d helped walk people through the valley of the shadow of AIDS during the darkest years of the crisis. I interviewed a nun who had served as the first female chaplain at Rikers Island, the city’s main jail complex, and had spent nearly a decade ministering to women with HIV; she thought she might know who the child was—but, in the end, she did not. I even managed to track down a former prison inmate who had dug graves on Hart Island as part of the Department of Correction’s burial detail—because graves were dug by inmates from Rikers Island for most of the cemetery’s existence. This man remembered the prayers he said for babies before burying them, but he knew nothing about SC-B1.
When I ran out of Hart Island leads, I played investigative reporter for a spell, filing a series of records requests with city agencies. My hope was that by following the long paper trail of death that accompanies each body to Hart Island, I might finally find my way to the child. But here, too, I hit only dead ends: The agencies I solicited—the departments of Correction, Health, Social Services, and others in the city’s surprisingly vast bureaucracy of death—either refused to produce the documents on privacy grounds or said they didn’t have them. In the case of one particularly critical set of records—a series of log books in which the DOC recorded all Hart Island burials—both of the agencies I solicited insisted the other one had them. The DOC, which ran the cemetery on Hart Island until 2021, said that “all data regarding burials, interments, and disinterments at Hart Island” had been transferred to the Human Resources Administration, which now helps manage the island; HRA, in turn, produced only a single set of burial records—and all the burials were adults. HRA said these documents were the only ones currently in its possession.
None of this surprised Melinda Hunt, an artist and advocate whom I came to think of as the guardian of lost Hart Island souls. Hunt had come across SC-B1’s grave during a visit in early 1992, when she and the photographer Joel Sternfeld were working on a photo book about the island, and I’m pretty sure she was the first civilian to learn about the child. “We were told by the correction officers that there was a grave, of a child who was the first child to die of AIDS in New York City, in this more remote location,” she recalled. “I think in their own minds, they felt that the grave should be documented, that it was special.” When Hunt and Sternfeld made their way to the spot, they found the marker, surrounded by weeds and vines, and snapped the first known photo of the grave.
Hunt was pregnant at the time, and the story of the child stayed with her. So when she started an organization called the Hart Island Project, which is dedicated, in part, to connecting the living with the dead—that is, the families of those buried on Hart Island with their lost loved ones—she made a point of keeping her eye out for information about SC-B1. In 2007, she filed records requests with the DOC for burial ledgers going back to 1985—and, after threatening to sue, she eventually got hold of them. But she couldn’t find any trace of the child when she combed through them. “I looked for SC-B1 in the baby listings because I wanted to know the name of the child long before you contacted me,” she said. She came to suspect that SC-B1’s burial information had not been recorded properly in a ledger.
I should probably have quit the search around this point, given up the reporting ghost, but obsession is a hard habit to kick. So, despite the dead ends—and a dawning suspicion that perhaps SC-B1 did not want to be found, or, at least, did not want me to be found by me—I kept reporting, kept interviewing. And while none of this got me any closer to solving the mystery of the child—in fact, I will just say it now: I never did find SC-B1—it did begin to yield other discoveries.
One of those discoveries was a man named Capt. Eugene Ruppert. Ruppert was in charge of Hart Island for the Department of Correction for nearly 20 years, from 1983 until 2000, and he was the person who oversaw the burial of SC-B1. “That was me,” he proclaimed during our first conversation. When I asked him about the log books, he assured me that SC-B1’s burial details had been recorded in one of them—and then e-mailed to specify that he believed the child’s burial details had been recorded in a special notebook, one that was not used for general burials but for AIDS burials. “I think it was a Notebook possibly soft cover. Remember it has been over 20 years since I was there.”
When I met Ruppert, he was 74, chatty, and bursting with Hart Island arcana—about the choreography of interment and disinterment (which, he said, happened roughly 10 percent of the time); about the decommissioned Nike missile site at the northern end of the island; about the tulips he said he had planted to prettify the place. I had high hopes that he might be my big reporting breakthrough. But of all the many things he could recall, the only thing it seemed he could not was the identity of SC-B1—not the child’s name, not their age, not their gender, nothing.
Still, there was one thing Ruppert was able to tell me: He was able to tell me who the child was not—and that information opened up a vast new universe.
SC-B1, it turned out, was not “Special Child–Baby 1,” as the Internet insisted. Instead, Ruppert explained, SC-B1 was “Special Case–Baby 1,” and that single word switch—from the saccharine sweetness of “special baby,” which suggested that this grave had been created as a kind of memorial, to the blankness of “special case”—proved to be important to understanding SC-B1’s story. “Special case,” it turned out, was an official term, a designation that Ruppert said the DOC used for a whole group of people who had died of AIDS and been buried on Hart Island between 1983 and 1986. These people had been placed in a special, segregated site—fenced off from the rest, in individual graves dug extra deep—out of an excess of caution at a moment of high fear of contagion. “I had a responsibility, not only to the officers that worked for me but also the inmates that did the burials, to prevent body fluids from people that died of AIDS,” Ruppert explained. There are as many as 35 of these other “special case” graves, and all of them, except SC-B1’s, belonged to adults.
Ruppert also had another big revelation. While various websites—from Wikipedia to National Geographic to the New York City government’s own Hart Island information page—had told me again and again that SC-B1 was the first child to have died of AIDS in New York City, Ruppert (along with others, eventually) made clear that this part of the SC-B1 legend was plainly false. Special Case–Baby 1 was not the first child to succumb to HIV in New York, not even close. In 1985, the year of SC-B1’s burial, the city’s Department of Health listed 27 children between the ages of 1 and 14 as having died of AIDS—a number that was almost certainly an undercount. And in the years immediately before, dozens of children had likely died from the disease. Far from being an outlier, Special Case–Baby 1 was a representative, an emblem—one of many children who had died of a sickness that had blasted families apart throughout the city.
When I was beginning my search, one of the first people I reached out to was a pediatrician named Elaine Abrams, who had worked at Harlem Hospital during the grimmest days of the HIV and AIDS crisis. As I explained my quest to her, I heard her inhale deeply before saying, “You are opening a door to a very big room. It’s not exactly a haunted house…”
Dr. Abrams didn’t finish the sentence, but as I attempted to trace the story of SC-B1’s life, as I revisited an era that so many had tried to move past, I found that the world she was describing was, indeed, haunted. And it was very, very big.

In the annals of HIV and AIDS history, the beginning of the epidemic is often traced to June 1981 and the release of a Centers for Disease Control report alerting the medical community to five cases of an unusual pneumonia in “previously healthy” gay men. In the months that followed, troubling reports piled up—including of a “rare and often rapidly fatal form of cancer,” Kaposi’s sarcoma, also in gay men—and soon medical experts were warning the world of “a new homosexual disorder.” They initially called it Gay-Related Immunodeficiency, or GRID, but by September 1982, they had come up with a new name for it: acquired immunodeficiency syndrome. AIDS.
Popular
“swipe left below to view more authors”Swipe →For many, these events have become synonymous with the start of the American epidemic, the moment the gun went off. But even before then, there were signs—clues picked up by a handful of people, both within gay communities and without: a strange and virulent pneumonia that was striking heroin users in New York; a sickness, which doctors dubbed “Rikers Island adenopathy,” that was hitting inmates in the city’s jail; and cases of immune-system collapse that were showing up in young children in clinics in the Bronx and Newark and a few other cities.
One of the first people to spot this last sign was an immunologist and pediatrician named Arye Rubinstein, who has worked for the past 50 years at the Albert Einstein College of Medicine. Rubinstein is an expert in immunodeficiencies—one colleague, at another hospital, described him as an “immunologic guru”—and this meant he was often the person whom other doctors called when they were stumped. This time, however, Rubinstein was also stumped. “We saw patients that we could not figure out what they had,” he told me as we sat in his living room, which was dense with plants and family portraits.
Rubinstein was 87 when we first met, with an enviable head of white-gray hair and a tendency to lapse into research-speak—into talk of epitopes and antibodies, B cells, T cells, and protein fractionation. I had first reached out to him in the hope that he might have insights into the mystery of Special Case–Baby 1, but he could offer nothing there—“I don’t know anything about this,” he said. He did, however, have another story.
In late 1978 or early 1979, a young child was referred to his clinic. This child was a boy—a fact I learned from a 1987 article in New York magazine, because medical privacy laws now prevent doctors from discussing details of their patients—and he was suffering from recurrent infections. Rubinstein took a case history and learned that the child wasn’t the only one in his family who was sick. His mother also had recurrent infections. She was a sex worker and an injection drug user, and she soon gave birth to another child who suffered from such severe illnesses—among them, bouts of septic pneumonia—that Rubinstein and his team considered giving the child a bone-marrow transplant. But they couldn’t find a donor, and before long, the baby died.
Rubinstein quickly began to suspect something unusual was going on, so he got to work in his lab, and what he found surprised him. All three family members were clearly suffering from an immunodeficiency, but it expressed itself somewhat differently in each. “We knew this is not a genetic disorder,” he explained. Instead, Rubinstein suspected they were dealing with a novel illness—a suspicion he noted in the last paragraph of the child’s chart notes, his colleague, Dr. Larry Bernstein, told me.
“I actually remember the very first patient that Dr. Rubinstein saw,” Bernstein said. “He described the immunological abnormalities in a handwritten note, and then he wrote ‘new immunodeficiency’ with six exclamation points.”
Rubinstein’s suspicions solidified into conviction over the next few years as additional children showed up in his clinic with signs of immune deficiency—failure to thrive, swollen lymph nodes, enlarged livers, pneumonia, recurrent infections. So when the CDC issued its first reports of a mysterious immune deficiency among gay men in 1981, they hit the Einstein team with the uncanny force of recognition. “I thought immediately: It’s related,” Rubinstein said. “It immediately turned on the light, and I said, ‘This is what we are seeing in children.’”
The problem was that few people outside of his clinic—and the one or two hospitals where other doctors had begun seeing serially sick children—believed him. The medical establishment remained unconvinced. “They thought it’s only affecting the gay community, and they would not accept something else,” Rubinstein told me.
In an attempt to nudge them toward acceptance, he submitted a paper to The New England Journal of Medicine about several children who showed signs of what he and his coauthors thought was a new immune deficiency, but the journal didn’t accept it. It wasn’t until mid-1983 that another publication, JAMA: The Journal of the American Medical Association, published his article alongside a report from another pediatrician, James Oleske, on eight cases of AIDS-like symptoms in children from Newark. While the articles didn’t get everything right, the fundamentals of what they described would prove devastatingly prescient: Children of poor Black and Latina women—many of them drug users, or partners of drug users, some of them sex workers, all living in communities that had been largely abandoned by the rest of the country—were being born with a devastating illness that looked strikingly similar to what was being seen in gay men.
Rubinstein’s and Oleske’s articles, along with the CDC’s own evolving research, helped push the medical establishment to acknowledge that children were getting sick with AIDS. And alongside that acknowledgment came the first drips of attention and resources. Rubinstein got a grant from the National Institutes of Health to study AIDS in women and children, ultimately discovering that the virus that causes AIDS can be transmitted to children in utero, through the placenta (the other two routes are during childbirth and through breast milk). He also began building up what would become one of the city’s largest programs to treat children with AIDS and their families.
But in many ways, by the time the broader medical world came to accept the reality of AIDS in children, it was already too late. The illness was steps ahead of the medical system, and the pediatric wards of New York’s public hospitals were filling up with children.
Dr. Stephen Nicholas was in the last year of his residency when he arrived on one of these wards, at Harlem Hospital, in 1982. He was a wide-eyed boy from Wyoming—tall, slim, soft spoken and very much committed to his cowboy boots. He was still figuring out his path but he was certain of one thing: He did not want to work with dying children. “I mean, who wakes up in the morning and says, ‘Boy, that’s what I want to do,’” he explained. But within a short period of time, that was precisely what Nicholas and a team of doctors at Harlem Hospital were doing. “It started as one, then it was two, then it was four, then it was—you know, this sort of progression,” he said. “I would say that by the end of the first year, we had dozens. And before long, we had a couple hundred.”

This period of the AIDS epidemic ushered in a truly monstrous moment in this country’s history. As the illness shifted from a medical curiosity to an epidemic, it revealed itself as a wily and relentless disease, one that killed painfully, almost sadistically, attacking the immune system from within until the body was left wholly exposed to attacks from without. There was no treatment at that time, nothing to slow or stop the illness ravaging the body, and, for a period, people didn’t even know how it was spread. Was it through sex? Casual contact? Any and all bodily fluids? It wasn’t until 1983 that scientists finally determined that it was triggered by a virus—one they eventually named the human immunodeficiency virus, or HIV—and it wasn’t until 1985 that they developed a test for it.
“It was an awful disease back then—they were just dying,” said Maxine Frere, a nurse who spent all 50 years of her professional life working at Harlem Hospital, much of it alongside both Stephen Nicholas and Elaine Abrams. Frere, who was born and raised in Harlem, grew up in the shadow of the hospital and knew from the time she was small that she wanted to be a nurse. “Doctors heal illnesses; nurses heal spirits and souls and everything else,” she explained. “Nurses take care of people.” Frere was taking care of kids in the pediatric ward when the first children with AIDS began arriving, in the early 1980s. They showed up with a range of symptoms—thrush and “fever of unknown origin” and that dispiriting catch-all symptom, “failure to thrive”—and the fear and uncertainty that swirled around this new sickness were so intense that many of Frere’s coworkers wanted nothing to do with them. Some wouldn’t enter the patients’ rooms. “They’d knock on the door and pass the food,” she said, describing how colleagues would slide trays of food through a crack in the door rather than bring them to the patients’ bedsides. “The nursing staff was afraid to touch HIV.”
Frere wasn’t afraid—or she wasn’t willing to let that fear stop her. When a doctor asked her if she wanted to begin working on AIDS-related clinical trials, she signed up. “I wanted to do the clinical trials,” she said, “because I wanted to make sure they were done correctly for my people, because those were my people, my neighborhood, my children.” AIDS had arrived in Harlem just a decade after the revelations about the Tuskegee experiment, in which white doctors deliberately withheld treatment from Black patients suffering from syphilis, and Frere was determined that nothing like that would ever be repeated on her watch. But she also had another reason for taking the job. “This was what I was supposed to do,” she said.

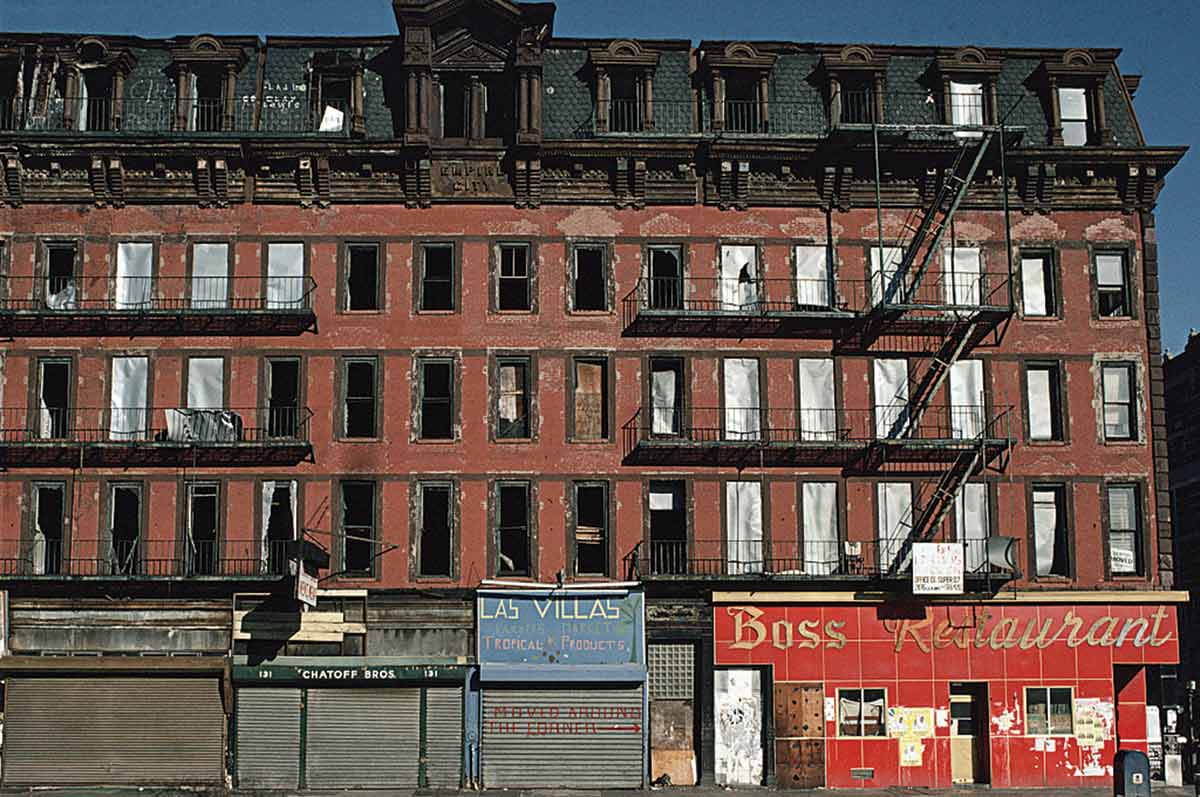
What Frere understood but so many others failed to see was that HIV was hitting Black and Puerto Rican communities with a battering force. These were neighborhoods like Harlem, the South Bronx, the Lower East Side, central Brooklyn, places where you could practically see the Federal Housing Administration’s red lines still glowing around their edges. It had been a bruising few decades for these neighborhoods—for all of New York, in fact, but for these communities in particular. They had suffered one blow after another. When the city’s manufacturing economy began to disappear in the 1960s and ’70s—the city lost a staggering 600,000 jobs between 1969 and 1976—it was working-class districts like these that endured some of the worst job losses. When the drug trade expanded into this breach, it was these neighborhoods whose streets were turned into open-air heroin markets and whose residents were then targeted by the new War on Drugs. And when New York City suffered a debilitating fiscal crisis in the mid-70s, and the city’s leaders embraced austerity, it was these neighborhoods that were marked for disinvestment. Now there was this virus, which was spreading through sex but also, crucially, through the shared needles people were using to inject heroin. And its emergence had everything to do with the collapse that had preceded it.
“AIDS was not just a medical crisis,” my colleague Kai Wright explains in the first episode of our podcast, Blindspot: The Plague in the Shadows. “It was and it remains a social disease, one that exploits the inequities that… define so much of American life.” It was, he says, “a systems-wide failure.
The numbers that began to emerge several years into the epidemic testified to this reality. In the late 1980s, researchers estimated that between 50 and 60 percent of New York City’s 200,000 injection drug users were infected with HIV, a stunning number that translated into harrowing case rates in several Black and Puerto Rican neighborhoods. In one 1988 study from the South Bronx, researchers estimated that 9.4 to 21.6 percent of men between the of ages 25 and 44 had HIV, while the rate for women in the same age range for women in the same age range was 2.4 to 5.5 percent.
What these numbers meant, in human terms, was that entire groups of friends and neighbors were getting infected—cohorts of young people who were simply disappearing. Sometimes, whole families fell ill as mothers, often unaware they had HIV, passed the virus on to their children during pregnancy, birth, or shortly after. At one hospital in the South Bronx, researchers reported that 5 to 10 percent of the women giving birth had HIV; in Harlem, a study found that 3 to 5 percent of the women giving birth were infected.
To be clear, not all of these women gave birth to children who were infected with HIV. Studies suggest that a little more than a quarter passed the virus to their kids, almost always without knowing, and the resulting numbers of children with HIV were never vast—nothing like the numbers of adults getting infected. But the pattern of illness that emerged during this period was nonetheless stark: One article from the late 1980s estimated that 90 percent of the kids with AIDS in New York City were Black or Latino.
And the world these children entered—the gritty, struggling New York of the 1980s—was largely unprepared to meet the challenge of the moment. “The kids were dying left and right,” Frere recalled.
From her perch at Harlem Hospital, Frere saw the shape of the AIDS crisis emerging early and understood its implications for the community where she lived, worked, and had grown up. So did her colleague Stephen Nicholas, even though he was newer to the neighborhood. All these decades later, he still keeps a photo of the first baby he treated who had AIDS, a little girl who arrived at the hospital in July 1983, 8 weeks old but already dying. The little girl’s mother was also young, only 22, and she too was sick. The photo is not easy to look at—it’s full of pain and has an intimacy that feels wrong to breach—so I will just say this: The little girl stares up at the camera with wide, slightly alarmed eyes, a red barrette in her hair and a slender tube taped to her nose. “She turned out to have pneumocystic pneumonia, which was the same thing that was being seen in adults with AIDS,” Nicholas said. She died not long after the picture was taken.
“So that,” he concluded, “was the beginning.”
In the months and years that followed, the story of this little girl repeated itself again and again on Harlem Hospital’s 17th floor, as well as at other city hospitals. There were differences among the cases, to be sure: Some children lived into their toddler years or even made it to the double digits before their immune systems gave out; others had mild cases that enabled them to make it, somehow, to the miracle era of antiretroviral therapy, which began in the late 1990s. But one theme that bound many of these children together was that they were dying alone.
Because HIV was inevitably a family disease in the cases where kids were concerned—spread from mother to child or sometimes from father to mother to child—one or both parents were always ill as well. Sometimes, they were so ill they couldn’t care for their kids or had already died; other times, addiction sent them into the streets and kept them there for days, weeks, or even longer; and all too frequently, mothers lost their kids to a foster care system whose solution to the drug epidemic was simply to take children away. This system then proved utterly unequipped to look after children with a stigmatized and often fatal disease.
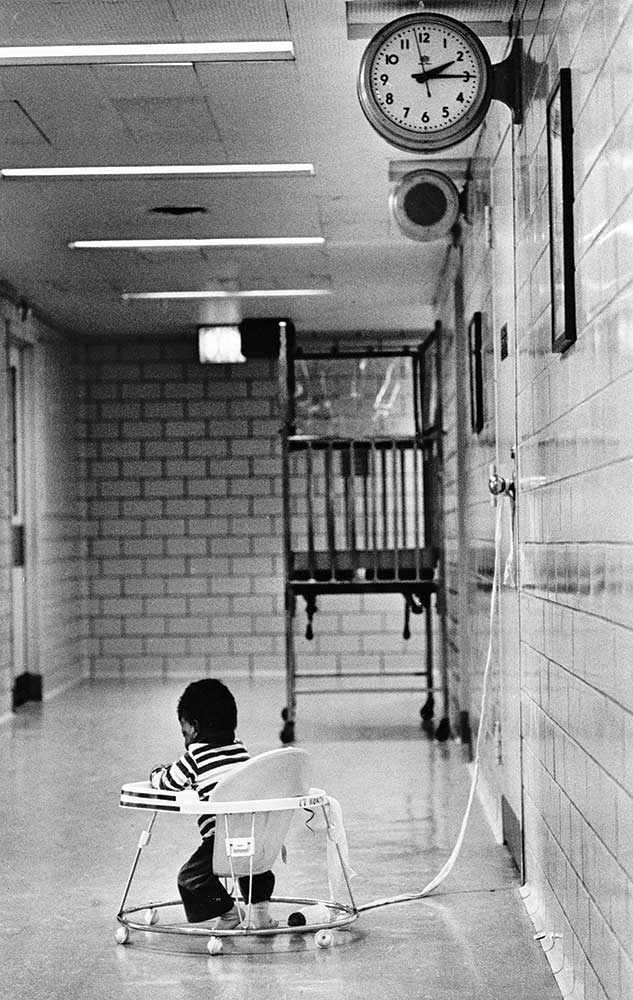
What this meant was that a number of children with HIV wound up sick and alone on hospital wards, spending months and sometimes even their entire brief lives there. “We had many children who lived in the hospital because they couldn’t go home,” Abrams said. By the mid-’80s, the problem had become so pronounced that someone, somewhere, came up with a name for these children: boarder babies. At Harlem Hospital, which became the home of necessity for more of these children than any other hospital in New York, the average length of stay, according to an article written by Nicholas and Abrams, was 339 days.
Within this bleak landscape—one where sick children lived out their days at underfunded hospitals, in communities that the wider city had abandoned—there were nonetheless acts of remarkable decency and goodness. There were people who stepped into society’s breach—nurses and doctors who held kids when others were scared, tasted their medicine to make sure it was palatable, celebrated their milestones. In several cases, nurses adopted their young patients. “We were a family,” Frere said.
Still, even in families, children sometimes fall through the cracks, and almost every time I asked a nurse or doctor to describe how a child like SC-B1 might have ended up at Hart Island, they shared some version of the boarder-baby scenario. “That child could be so many different children from all over New York City. Particularly in the Bronx, parts of Brooklyn, and Harlem, there were children dying from HIV who were nameless, who had no family, who could be that little boy or little girl there,” Abrams told me. “There were many children like that—not hundreds and hundreds, but there were babies like that.”
Like several other doctors I spoke with, Abrams had specific children in mind—a little girl who “had no visitors, or maybe one visitor, over the course of many, many months,” she said. “She just was a ward of the state.” Abrams didn’t know where she was buried after she died, but she wondered. And when I asked Nicholas about the possibility that children from Harlem Hospital’s 17th floor ended up at Hart Island, he said that, early on, a nurse had told him that some of the children who died alone were buried in the potter’s field. But “once we became aware of that,” he said, “the nurses at the hospital oftentimes would pool money to make sure that the baby got a funeral.”
Frere doesn’t recall any children with AIDS getting buried on Hart Island—certainly not on her and her colleagues’ watch. “Maybe before we all started,” she said. But after that, “I can almost swear that no kid who died in Harlem went to potter’s field.” Instead, she remembers staff chipping in to help with burials. “People would give their grave sites and buy the clothes and everything for them to be buried.”
There were other possibilities, of course, other scenarios by which a small child who died of AIDS might have found their way to Hart Island: they might have died surrounded by family, but that family couldn’t then afford the high expense of a burial; or perhaps that family couldn’t find a funeral home that would prepare the body and arrange the burial, as was all too common in those days. In 1983, the New York State Funeral Directors Home advised its members not to embalm the bodies of people who had died of AIDS.
Still, the grim truth is most of the doctors and nurses I polled suspected that SC-B1 had died alone in a hospital—at Jacobi or Lincoln in the Bronx, Bellevue or St. Vincent’s in Manhattan, Kings County Medical Center in Brooklyn—or any number of others—with no family to usher it to its final resting spot. “There were so many of these really special little kids who didn’t have the luxury of a home,” Abrams said, “or, really, a life.”

This story could end here, in the lonely corner of an underfunded pediatric ward, in a city that was unprepared to meet the challenges of a deadly new virus. And yet, if the story did end here, it would be incomplete. It would be a story that described only who Special Case–Baby 1 might have been—and not who they could be, even now, if HIV had moved slower and the world had moved faster. It would be a story only of death, when the story of pediatric AIDS is also, ultimately, one of life.
In 1996, more than a decade after SC-B1 died, a mother waited outside her daughter’s room at Bronx-Lebanon Hospital. This mother was Michelle Lopez, and she was still baby-faced at 29, still carrying traces of Trinidad, where she grew up, in her voice. Her daughter, Raven, who was 6, was in the hospital as part of a clinical trial for a new drug to treat HIV—a protease inhibitor that was being developed, for the first time, to give to children as well as adults. Lopez was anxious.
“I had friends of mine who were like, ‘Michelle, you’re crazy. They could kill your kid,’” she told me recently, her voice rising to a taut squeak. “But,” she recalled, “I looked at them, and I said, ‘What more does she have to lose?’”
Raven had been diagnosed with HIV in 1991, when she was roughly a year old, and by this point her immune system was buckling. She had bouts of pneumonia and frequent ear infections; one doctor had told Lopez that Raven probably wouldn’t make it to the age of 7.
Lopez was also sick. She had been infected before Raven was born, by Raven’s father, she believes, and like far too many women during that era, she hadn’t known she had the virus when she was pregnant—hadn’t even known she was at risk of getting it. She had found out only after she had fled with Raven to a domestic violence shelter, where a caseworker suggested that she, and then Raven, take a test. HIV was still a death sentence at this point—in 1990, AIDS was the leading cause of death for Black women in New York State between the ages of 15 and 44—and the discovery that both she and her daughter had the virus could easily have pushed Lopez to give up.
“We had no guidelines for us as mothers. We were left to raise this child that was born with this disease. Every day was traumatic for me,” Lopez recalled. “But,” she added, “I learned from [my] communities, you’ve got to do what you’ve got to do to save this child.”
One of those communities was ACT UP, the fiercely inventive AIDS activism organization that was formed in 1987. Lopez had been connected with the group by her caseworker, and the activists “really embraced me,” she said. They “mentored me, protected me”—and, she said, they “motivated” her, tapping into what would turn out to be a gale-force activist spirit.
In the months after her diagnosis, Lopez became a hurricane—advocating, agitating, and pushing to expand the terrain of rights and resources for people with HIV. “I kept going. I kept giving myself up to do a testimony, to be a claimant,” she said, describing how she spoke at conferences, testified for legislation, joined lawsuits. Her mission was to create the support structures that would allow her daughter and her, as well as the many parents and children in situations painfully similar to theirs, to survive: the affordable housing for people with AIDS, the medical care for pregnant mothers, and, above all, the treatments for children, who were largely being ignored by the pharmaceutical industry. It was this last quest that ultimately convinced her to sign Raven up for the clinical trial for the new protease inhibitor, which included a 24-hour dosing test to determine the proper amount of the drug to administer to Raven and other children.
“We were praying,” Lopez said of the day of the dosing test. “That’s all that I remember—prayers.”
The trial did what it was supposed to do, it was successful. Raven made it through the study, unscathed and unshaken, and then stayed on the drug through its approval by the FDA in 1997 and beyond. It was a landmark moment in the history of pediatric HIV and AIDS. Viracept, as it was called, was among the first successful treatments for children with the virus, and it transformed not only Raven’s life but the lives of other HIV-positive kids throughout the United States. Alongside another critical intervention—the discovery in 1994 of a therapy to interrupt the transmission of HIV from mother to child during pregnancy—it heralded the beginning of the miraculous, albeit slow and still unfinished, end of the pediatric HIV and AIDS crisis in this country.
Raven “really, really made a great impact for pediatric AIDS in reference to children having access,” Lopez said. “And,” she added, “it was a little Black girl from the Bronx.”
Lopez was sitting in Raven’s apartment when she told me this, perched next to her daughter on a black couch decorated with a single sparkling silver pillow. Lopez is 57 now, with electric energy and a full-bodied laugh. She is still protective of her daughter, still determined to tell the world what the two of them survived, and how.
Raven is more subdued: As her mother spoke, retelling this essential moment of family and medical lore, she seemed proud but also weary, perhaps because she’s heard the story so many times before, or perhaps because it feels oddly disconnected from her own memories of her life. She remembers the day when she was 6 that she learned she had HIV; remembers being afraid that she would die; and remembers her doctor’s reassurances. But the clinical trial that saved her life, as well as her many trips to the hospital—the poking, the prodding, the appointments—are lost to her. “I don’t remember all of that process,” she said.
Raven is now 33, which means that she has outlived the medical establishment’s dire early predictions for her by decades. Her life is, in many ways, a miracle. She now takes one pill once a day to suppress her HIV, and has a child of her own—a 6-year-old son who is HIV-negative and is the joy of her world as well as her mother’s. On the day we met, she was dressed in the saturated pink hues of a Barbie top, her hair accented pink as well. “I’m a pink girl,” she said. “If it was up to me, the world would be pink.”
Even so, Raven will be the first to say that the arc of her life has not been a smooth one. Much like her mother—and often right alongside her—she had to fight at each step and juncture of her journey, pushing back against the ignorance and stigma of her classmates, weathering moments of fear and despair. In elementary school, there was the teacher who refused to let her use the bathroom or go on school trips; in high school, there was the boy who told everyone she had “the Monster.” Throughout her life, there have been the friends who have died from the illness she has survived. “It was hard for me growing up,” Raven said.
Still, she prefers to focus these days on the fact of her survival, on life. “I got to show people: ‘Look, I’m that girl that’s still here!’” she said.
As we prepared to part ways, I decided to broach the subject of Special Case–Baby 1, to ask Lopez if she could imagine the child’s story, and if she thought it could tell us something even today. She didn’t pause. “These women and children back then did not have the kind of infrastructure we built… the community that I discovered and embraced me,” she said. “Those women and children did not have that in the early ’80s.”
It’s among the reasons she felt she needed to fight so hard. “They were not on the radar, or they were not a priority identified by our public health system,” Lopez said. “They fell through the cracks.”

On a bright but bitter day in November 2022, I stood in a clearing ringed by spiny trees at the southern tip of Hart Island, staring down at the grave of Special Case–Baby 1. It was my first trip to the island, and the grave looked more or less as I had seen it in pictures, an unobtrusive slab of concrete that could easily be mistaken for a mile marker if you didn’t know better. The island itself looked different than I’d expected—not a haunted place of decay and lurking ghosts, but a serene landscape of pale green and brown that seemed almost to hover above the water. It was handed over to the Parks Department in 2021 and cleaned up, the weeds pulled, the grass trimmed, the crumbling buildings torn down. The place was magical. From its shores, the city looked only half-real.
I had managed to score permission to visit Hart Island through my work with WNYC—reporting on HIV/AIDS for Blindspot—and I was joined by three colleagues and Eugene Ruppert, the retired DOC captain who oversaw burials on the site. We had asked Ruppert to come along as our guide, and he obliged by gamely pointing out every structure, still standing or not, on our way to SC-B1’s grave—the site of the old laundry building, the pumping station for sewage, the place where an old schoolhouse had once stood. When we finally arrived at the grave, I stood for a few moments, not quite sure what to do, then stretched out my hand to touch the marker, hoping to convey reverence—or maybe, if I’m honest, to intuit something. Mostly, though, I intuited cold.
This was still early in my quest to find SC-B1, and I hadn’t yet lost faith that I could solve the mystery of the child’s identity. So I peppered Ruppert with questions, searching for ways to dislodge any memories of the day of the burial, but those memories had either never embedded or had long since been washed away. “We got babies every day,” Ruppert said. “We got stillborns, we got body parts, we got adults.”
“It was routine,” he continued. “It’s just what we did. It’s like driving a bus.”
As I left the grave site, I felt the first lurch of disappointment, but now I think I am relieved. More than 15 months after I began trying to track down Special Case–Baby 1, and 15 years after I first became fascinated with their story, I’ve stopped dreaming of finding out who this child was, stopped wanting to peer into the depths of this one human’s tragedy. Although I may not have uncovered the specific contours of SC-B1’s death—or their life—I do have a sense of its shape, and it is as bleak and intimate as any I could have imagined. It is the little boy who first showed up at Arye Rubinstein’s immunology clinic, and the little girl who died on Stephen Nicholas’s early watch, and it is any number of other children whose stories I have not told but will inhabit the sadder quadrants of my heart for a long time to come. After so much pain, crammed into such a brief life, it seems to me that whoever SC-B1 was, they deserve to rest.
I didn’t fully recognize the importance of this rest when I began my search. When I set out to find SC-B1, I was voracious in my determination not only to understand how a child with AIDS could have ended up on Hart Island—alone, in a segregated spot—but also to give the child a proper burial of sorts, to do them justice through the retroactive magic of words and storytelling. What I didn’t realize at the time is that the child already had a proper burial—a grave site, however troubled its origins, that is as peaceful and hallowed as any final resting spot. Nor did I understand that the nothingness of anonymity, from which I had felt such a strong need to rescue the child, was not an injustice—although it clearly started as such—but a shield. AIDS activists had fought since the very earliest days of the epidemic for the rights to privacy and confidentiality, for the ability to protect themselves from the world’s stigmatizing gaze. I would not want to be the one to strip that protection from this child.
“The point of a cemetery,” said Melinda Hunt, the Hart Island advocate and activist who first brought attention to Special Case–Baby 1, “is that it’s a communal reconciliation of death.” It is “where we keep our history”—and the way we tend to that history matters. This makes sense to me but it also raises a question: How do we possibly begin to reconcile a death like that of SC-B1? How, in fact, do we reconcile so many of the deaths of the AIDS era?
When I asked Michelle Lopez this question, she had a ready response: “We honor [the child] by…continually advocating,” she said. She reminded me that the HIV/AIDS epidemic is far from over, that people continue to get infected and die to this day, both in the United States and abroad. And so, she said, we must continue to fight—for treatments and for access to treatments and for a real cure—so that no one has to go through what she and Raven endured. Or what Special Case–Baby 1 did.
Nearly 40 years ago, a child died in New York City. This child died of a virus that snuck into the city’s veins and arteries, then made its way, undetected, down its willfully neglected streets and into the bodies of whole communities. This child was not the first one to die of AIDS, nor would they be the last; they were not the only special child—although they were special.
When this child died, their body was taken by ferry to an island-cemetery off the coast of the city. Because of the virus that killed them, the men who buried the child were afraid, so they carted their coffin to a fenced-off area that was separated from the rest. They lowered the pine coffin into the ground using a system of ropes, then left those ropes in the grave, along with their gloves and protective gear, and closed up the hole. Then they walked away, leaving the child in the place where it lies to this day—in a quiet clearing, near a stand of slender trees, beneath a marker that is only half-deciphered.
More from The Nation

A Civil Rights Veteran Revisits the Summer of 1965 A Civil Rights Veteran Revisits the Summer of 1965
The white college student supported Black voters in segregated Alabama, and began documenting the front lines of the voting rights fight, which locals continue to disregard.

Notes on Transsexual Surgery Notes on Transsexual Surgery
An abundance of plastic surgery is not a net good. But discussions over its morality would be better off viewing it less as unfettered desire and more as self-determination.

I Led the FDNY. Don’t Believe Elon Musk’s Nonsense About It. I Led the FDNY. Don’t Believe Elon Musk’s Nonsense About It.
Musk’s attack on the new FDNY commissioner proves he knows nothing about how modern fire departments work.

What Black Youth Need to Feel Safe What Black Youth Need to Feel Safe
Young people are facing a mental health crisis. This group of Cincinnati teens thinks they know how to solve it.

Trump’s Death Eaters Are Coming for Our Kids Trump’s Death Eaters Are Coming for Our Kids
After taking countless lives around the world, RFK Jr. and his ghoulish compatriots want American children to suffer too.

The Supreme Court Just Held an Anti-Trans Hatefest The Supreme Court Just Held an Anti-Trans Hatefest
The court’s hearing on state bans on trans athletes in women’s sports was not a serious legal exercise. It was bigotry masquerading as law.