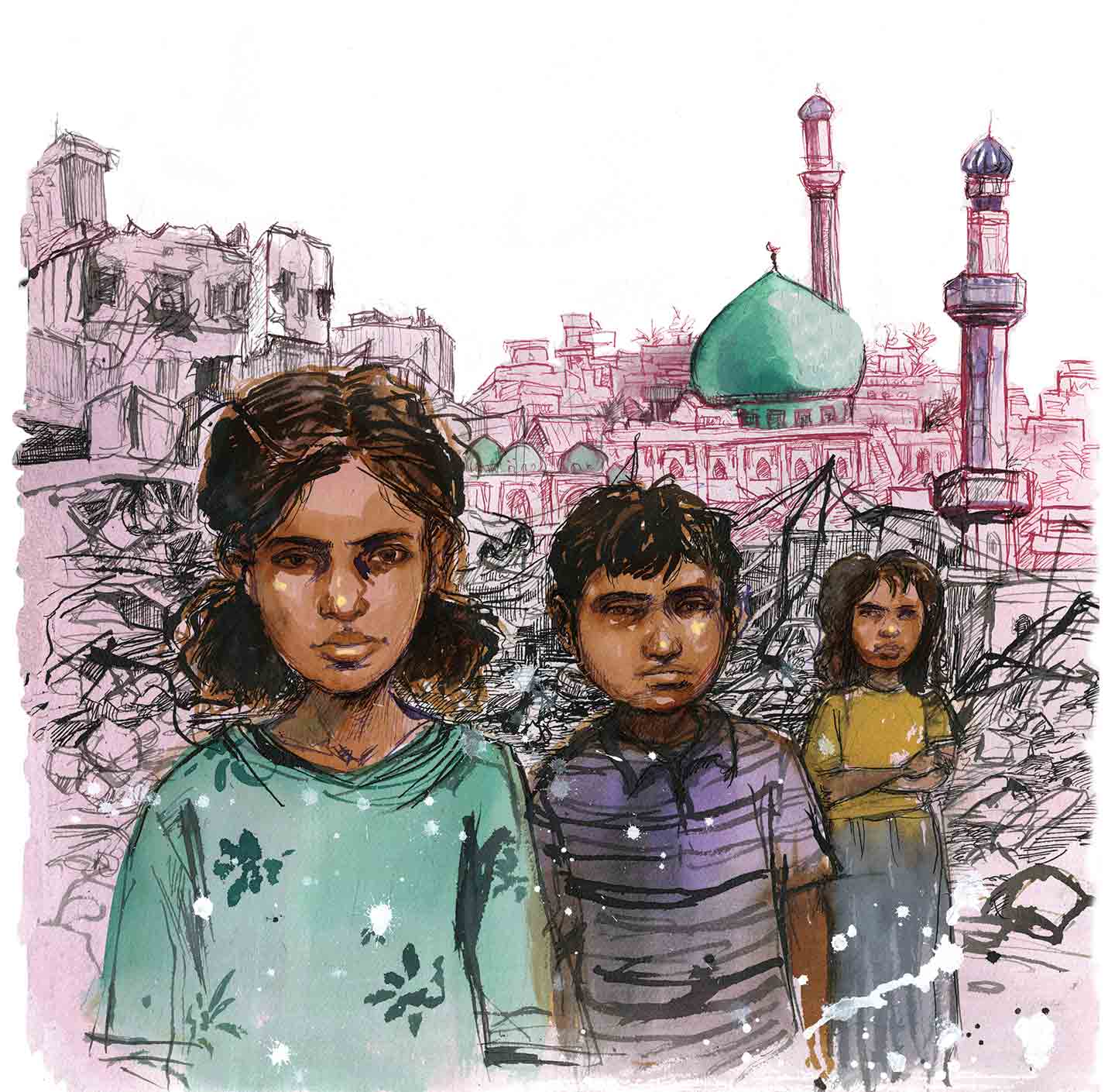
Three years after American soldiers besieged her city, Iraqi pediatrician Samira Alani began to see a problem in the maternity ward. Women were bearing infants with organs spilling out of their abdomens or with their legs fused together like mermaids’ tails. Some looked as if they were covered in snakeskin. Others emerged gasping, unsuccessfully, for air. No one knew what was wrong with the babies, although almost no one was trying to find out, either. It was 2007, the height of the political and sectarian violence unleashed by the US invasion and occupation. Fallujah, where Alani lived and worked, was considered one of the most unstable and inaccessible cities on earth.
The news about the babies spread from the hospital corridors to the inner courtyards of the city’s homes, whispered among female relatives and neighbors. Entisar Hussein, a housewife in Fallujah, learned about the deformities after a cousin returned from the maternity ward. “One woman, she had a child with a tail, and one, she had a child with a rabbit’s face,” Hussein recalled her cousin telling her. The sickness crept into Hussein’s family, too, she said: One of her sisters-in-law delivered an infant without skull bones to protect the brain tissue; the baby died at birth. Another sister-in-law had two miscarriages and then gave birth to a child with an enormous, bloated head. He died, too.
Soon Fallujah’s children became a topic of concern at tribal meetings and in the provincial doctors’ union. Many residents suspected that the major American offensives against the city might have had something to do with the deformities. The second offensive, which began in early November 2004, was the deadliest battle of the entire US war in Iraq—a six-week siege that killed thousands of Iraqis and dozens of Americans and left much of the city in rubble. But these suspicions were kept quiet. Outside people’s homes, just beyond the iron front doors, US Marines patrolled the streets, and residents said they feared the United States wouldn’t respond kindly to insinuations of having sparked a public health crisis. Moreover, the Americans weren’t the only actors that Fallujans had to consider. The Shiite-led national government in Baghdad, which many viewed as a puppet of Washington and Tehran, was engaged in a campaign of arrests, torture, and political retribution against its critics, particularly in Sunni-majority areas like Fallujah. In Fallujah, various Iraqi parties and militias were jockeying for political power, and they, too, sought to control the spread of information for their own agendas.
But even if people hadn’t been afraid, doctors and residents said it didn’t seem there was much anyone could do about the birth defects in those days. All across Iraq, the US invasion had unleashed a wave of violence against doctors, whose relative wealth and high profiles made them easy targets amid the country’s growing sectarian strife. By 2007, when Alani began to notice the birth defects in Fallujah, the Iraqi Medical Association estimated that half of registered doctors had been forced to flee the country. Those who remained, like her, risked not only arrest, kidnapping, and assassination but also the reality of straitened working conditions, brought on by shortages of drugs, medical equipment, and both water and electricity.
Popular
"swipe left below to view more authors"Swipe →“We felt that there was something wrong,” she recalled. “But we could do nothing.”
Alani’s colleague Muntaha Alwani, a fetal medicine specialist, also believed there was a problem. Both women have worked at the hospital since the late 1990s, and they thought they were seeing far more defects than before the US invasion. Alani quietly began to record the cases, and Alwani photographed the tiny patients. Alani made a form to register birth defects and distributed it across the hospital’s wards. Many of their coworkers were skeptical. “Some thought it was of no use,” said Alani. “Of course, they were wrong. Through our documentation, we brought the attention of the whole world.”
Alani’s ad hoc registry was the beginning of a yearslong, unfinished quest to document and investigate the most controversial medical mystery of the Iraq War: an alleged increase in birth defects that, local doctors say, began after the United States invaded the country in 2003 and plagues the city to this day. At stake is the question of whether US military activities in Fallujah contributed to these congenital disorders—an explosive possibility that has transformed this local public health concern into an international political and scientific controversy. For years, the fierce debate over Fallujah has centered on questions about the use and impact of potentially toxic material in US weapons, particularly depleted uranium. The discussion has largely overlooked, however, broader and perhaps even more troubling questions about the long-term public health effects of urban warfare on civilian populations and the dangers of politicizing science and medicine in times of conflict.
The Department of Defense did not respond to most of the questions posed by The Nation about allegations of rising numbers of birth defects in Fallujah resulting from the war. It did share its “Policy for Environmental Remediation Outside the United States,” which states that “DOD has no general authority or funding to engage in environmental remediation outside of the United States.” The policy also states that the Department of Defense “takes no action to remediate environmental contamination resulting from armed conflict.”
For its part, the Iraqi government said the United States has provided invaluable resources in addressing the country’s environmental and health concerns in the years since the invasion. “The United States support[s] us…not only in the field of radiation but also in the field of climate change and the pollution of the water resources,” said Jassim Abdulaziz Humadi Alflahy, Iraq’s deputy minister of health and the environment.
Still, more than 17 years after the US invasion, the mystery of Fallujah’s children continues to haunt Iraq. Nearly every aspect of the story of the city’s birth defects remains contested. And although accounts and images of Fallujah’s maimed and ailing children have traveled from the halls of the World Health Organization and the pages of medical journals to the text of internal Pentagon memos and the posters of anti-war marches, Alani and her colleagues continue to operate in a tiny and underresourced birth defects center, now treating children whose parents were children themselves when the United States invaded Iraq.
On a hot September morning in 2019, more than half a dozen women waited outside a squat building at Fallujah’s maternity hospital on the banks of the Euphrates River. Some sat alone, holding their children or grandchildren on their laps. Others milled around, greeting each other with kisses on the cheek. Among them was Samira Ahmad, who said her infant granddaughter, Maram, had been struggling to breathe since the family took her home from the hospital a few months earlier. She said that Maram is her daughter-in-law’s first child after two previous pregnancies ended in miscarriages. Later that day, the pediatric cardiologist discovered a small hole in Maram’s heart.
Alani, meanwhile, was driving from her house in the center of Fallujah to the hospital. As she drove, she passed clothing stores and vegetable shops, a shiny new burger joint, and roadside tea stands where old men kept watch over boiling kettles and dainty istikan glasses. Late summer is date season in Iraq, and platters piled high with the sweet fruit were perched on nearly every street corner. Scaffolding surrounded some of the famed mosques, whose minarets were punctured with bullet holes.
Alani’s daily commute hadn’t always been this smooth. In 2005 and 2006, after US forces occupied Fallujah, the streets were so choked by US military checkpoints that she had to travel the two miles from her home to the hospital on foot. In early 2014, she anxiously drove past masked fighters with the Islamic State on her way to work. Her home and her hospital have been bombed repeatedly. And yet then, as now, Alani was undeterred.
Shortly after 8 am, Alani parked in front of the birth defects center. A tiny, angular woman, she tilts forward as she walks, giving her the perpetual appearance of being impatient to arrive. She unlocked the clinic and then hurried with short, deliberate steps across the yellowed grass, past the men smoking cigarettes while awaiting news of their wives, and into the neonatal ward, where she bent over a child named Muhammed. He had been born two weeks earlier with a large sac containing part of his brain protruding from the back of his skull, according to a hospital photograph. This defect, called encephalocele, has a high fatality rate, but the doctors on duty said he was recovering from the surgeries that removed the sac and drained the excess spinal fluid.
Alani bent over the incubator, lifting Muhammed’s arms and legs and examining his short neck and misshapen ribs. “He will be crippled,” she said matter-of-factly. He was one of four babies with congenital disorders delivered in the facility on August 28, according to hospital records and interviews with doctors. Two were twins—one with a bloated head and the second with distorted limbs and abnormal genitals. The fourth baby had fully blocked nasal cavities; days earlier, she lay in an incubator next to Muhammed, crying as she struggled to breathe.
Alani cast about the crowded room for Muhammed’s grandmothers, who had stayed by his hospital bedside since his birth. “There are four babies and one, two, three… eight women in here,” Alani muttered to herself with a frown. “It’s not good for the babies.”
Alani has a brusque bedside manner that’s exacerbated by her various pet peeves—too many women crowded into a neonatal ward, doctors who hawk baby formula on behalf of milk companies, and worst of all, colleagues who refuse to participate in her beleaguered birth defects registry. Two decades earlier, she had fallen in love with pediatrics during her medical school training in Baghdad, and she has dedicated her life to the profession ever since. Five days a week, she heads to work in Fallujah’s public hospital, even as friends have fled to the capital or abroad or opted to spend the majority of their time in private practice. Still, after more than 20 years on duty, she occasionally wishes she’d chosen to specialize in dermatology or radiology or anything other than caring for children in a city seemingly plagued by unexplained birth defects.
After examining Muhammed, Alani headed to the hospital’s archives to track down the file for a patient who was born a few days earlier without a skull but whose case hadn’t been recorded in her registry. After some searching, she found the child’s documents amid the bundled stacks of pink, blue, and white sheets of paper. The family was from Abu Ghraib, about 20 miles east of Fallujah and home to the former US prison that became infamous for the torture and sexual abuse that American soldiers carried out behind its walls. She then returned to the birth defects center to examine a child diagnosed with Pierre Robin syndrome, a rare condition in which an infant has an underdeveloped jaw that causes breathing and feeding problems.
“Will she be normal?” asked the child’s grandmother Nahida Sami Aghul. She said it was the second time her daughter had a child with congenital defects; in 2014 she delivered an infant with a shriveled head who died.
“Probably not,” Alani responded flatly, warning that infants with this disorder can die from respiratory problems.
“We’re afraid of the next pregnancy. Can this happen again?” Aghul wondered.
Alani didn’t have an answer, and soon she was summoned back to the neonatal ward to examine a newborn whose spine protruded from a blood-red hole in his back. His mother was still in the delivery room, and she didn’t yet know about the infant’s condition. His grandmother hovered over the incubator and worried aloud about not having the money to pay for the baby’s treatment. Muhammed Namiq, another pediatrician, peeked into the room from the hallway.
“We have many cases like this,” he said.
This was his first year in this hospital, after stints outside Baghdad and in the country’s north and southeast. He said he has seen more birth defects in Fallujah than anywhere else he has worked. He pulled out his phone and showed a picture of an infant born in the hospital that year, according to records from the birth defects clinic. The child had no nose—an extremely rare condition known as arhinia.
Namiq said he performed surgery on the patient, but it didn’t work. The child died after the operation. According to the medical literature, only a few dozen instances of this condition have been recorded worldwide.
Over the past century, veterans and civilians across the world have voiced recurring fears about the health impacts of war on future generations. Conflict has, of course, always posed risks to public health. But the rise of industrialized warfare in the 20th century, with the introduction of chemical weapons and the threat of nuclear attacks, brought new toxic exposures and the possibility of terrifying genetic consequences. In August 1945 the United States dropped atomic bombs on the Japanese cities of Hiroshima and Nagasaki, killing more than 200,000 people and thrusting the world into the nuclear age. In the wake of the bombings, “public concern focused more on the genetic consequences than any other untoward health outcome,” observed the geneticist William Schull, a member of the US government’s Atomic Bomb Casualty Commission. “Many individuals had visions of an epidemic of births culminating in misshapen monsters or infants condemned to early death.”
Since then, modern warfare’s potential to deform future generations has sparked unparalleled attention and controversy, even as the science has rarely been conclusive. The largest longitudinal study of Hiroshima and Nagasaki survivors and their children was undertaken by the Atomic Bomb Casualty Commission and its successor, the US-Japanese Radiation Effects Research Foundation. After examining more than 75,000 newborns in Hiroshima and Nagasaki, RERF concluded that “no statistically significant increase in major birth defects or other untoward pregnancy outcomes was seen among children of survivors”—a conclusion reinforced by the agency’s subsequent studies. Despite these findings, the fear of mass genetic distortions sent shock waves through the scientific world and inspired epidemiologists to establish some of the first major registries of congenital disorders.
That fear radiated into the broader population as well. In the decades that followed, US veterans who participated in the Pentagon’s mustard gas experiments during World War II raised concerns about infertility and birth defects among their children. So did veterans sent to the Marshall Islands in the late 1970s to clean up the toxic waste from the Pentagon’s relentless nuclear testing, as well as Marshallese civilians who say the radioactive fallout from 67 nuclear bomb explosions has produced so-called jellyfish babies. In all three cases, the US government does not consider there to be sufficient evidence to link these tests with birth defects.
Then, in the late ’70s, the US public was confronted with prime-time television exposure to these nightmarish visions, as veterans of the Vietnam War began to report birth defects in their children. They blamed the disorders on their wartime contact with the herbicide Agent Orange, which the US Air Force sprayed across swaths of South Vietnam. “We’re not the veterans,” former Green Beret John Woods testified at a 1979 congressional hearing. “Our kids are the veterans.” Meanwhile, the Vietnamese Association for Victims of Agent Orange says as many as 3 million civilians across four generations have suffered from cancers, neural damage, reproductive problems, and other illnesses linked to the toxic chemical. Even now, Vietnamese officials say they are witnessing an increase in the number of children born with birth defects—four decades after the war’s end.
As in the earlier instances, the US government has disputed these claims, arguing “there is inadequate or insufficient evidence of birth defects…resulting from tactical herbicide exposure.” But a number of US and international studies have suggested a link between the chemical and some types of birth defects, helping fuel decades of debate.
Part of the challenge is the complexity of the science. “They [birth defects] are so damn hard to study and to understand and to get causal mechanisms,” said Leslie Roberts, an epidemiologist at Columbia University who has worked with the WHO. “And this makes them uniquely inflammatory and unresolvable. Sometimes we’ll have an issue like Agent Orange where we can actually measure chemical markers of exposure, but usually not.”
Compounding these scientific challenges are the sweeping financial and legal implications of any conclusive evidence. “We have enormously sophisticated propaganda machines that are trying to avoid any liability issues,” said Roberts. In the case of Agent Orange, US veterans sued the chemical companies that manufactured it, including Dow and Monsanto, and won a $180 million settlement in 1984. They also pushed the VA to cover health care for their children born with spina bifida and, in certain instances, a number of other birth defects, even as the agency maintains they are not related to Agent Orange exposure. Meanwhile, US veterans who were exposed to the herbicide and their children, as well as Vietnamese civilians and their descendants, continue to demand additional recognition and compensation for damages.
In 2008 a US court dismissed a class action lawsuit filed on behalf of Vietnamese civilians, after Seth Waxman, who served as solicitor general under Bill Clinton, argued on behalf of the chemical companies that the case could have far-reaching political implications. “This does affect our ongoing diplomacy,” he said. The diplomacy he was referring to was not abstract but was related to a specific conflict that was being fought some 6,000 miles away, with its own controversial weapons: the war in Iraq, during which the US was rumored to have used depleted uranium.
In Fallujah, more than a decade after Alani set up the hospital’s birth defects registry, the issue of congenital disorders remains politically controversial and scientifically disputed. As Fallujah’s doctors see it, on one side of the debate are Alani and her colleagues as well as doctors from across Iraq, most notably in Najaf, Nasiriyah, and Basra, who all contend they are facing a crisis of birth defects; on the other are the world’s most powerful medical and military institutions—the WHO and the Pentagon.
Alani and her colleagues maintain that the prevalence of congenital defects in Fallujah has been troublingly high in the aftermath of the 2003 invasion. To prove that this is more than just anecdotal observation, she set out in 2009 to track every birth defect case referred to one of the three pediatric clinics at Fallujah General Hospital over 11 months. Her study, published in the Journal of the Islamic Medical Association of North America, found that an estimated 14 percent of infants delivered at the hospital had congenital disorders—more than twice the global average.
It became one of Alani’s most widely cited studies, despite limitations in the data. As she acknowledged in the paper, she lacked precise information for the number of cases referred to the clinic, forcing her to estimate. Bernadette Modell, an emeritus professor of community genetics at University College London and a longtime WHO researcher, said Alani’s study suffered from a challenge facing most clinicians working in resource-strapped or conflict settings: a lack of reliable epidemiological data. “This is a sincere effort, but it does not provide definitive evidence,” said Modell.
Still, Alani’s findings were supported by other small studies conducted by her colleagues, including one by Alwani. And former Iraqi government ministers and top health and environmental officials told The Nation that Fallujah has experienced a disconcerting increase in the prevalence of birth defects since the US invasion (although they did not provide government studies corroborating their statements).
In 2013, however, a national survey conducted by the Iraqi Ministry of Health and supported by the WHO reached a dramatically different conclusion than Fallujah’s doctors did. Based on interviews with residents in 18 of Iraq’s more than 100 districts, the survey concluded, “The rates for spontaneous abortion, stillbirths and congenital birth defects found in the study are consistent with or even lower than international estimates.” In Fallujah, it determined, the prevalence was half that of rich countries.
The discrepancy between Alani’s findings and the Health Ministry’s WHO-backed survey ignited a scientific firestorm that continues to smolder.
Modell said she thought the 2013 study was well conducted, given the challenges in carrying out large-scale epidemiological studies in conflict zones. “When I looked at the methodology, it was very, very impressive,” she said. But other experts—both Iraqi and international—criticized the survey for being prone to a number of flaws, including recollection bias, since it was based on parents’ memories of stillbirths, miscarriages, and birth defects, rather than hospital records. (The study recognized the “possibility of recall error” as a limitation in the methodology.)
“There must be underreporting. That’s quite clear,” said Jon Pedersen, an independent consultant who has worked on infant mortality surveys with the United Nations and other international agencies, particularly in the Middle East. (Modell and Pedersen participated in a 2013 meeting with Iraqi officials in Geneva to review the survey’s data before the report’s publication.) The debate garnered such heat it spilled into the pages of The Lancet, one of the most prestigious medical journals, where a number of doctors, including Alani, criticized the study for everything from its methodology to its scope to failing to meet the standards of peer review.
The controversy was as much about politics as about science. When Alani and other Fallujah hospital doctors questioned the study’s methodology before its release, Alani said, they were accused by members of the US-backed Iraqi government of manipulating the medicine to manufacture anti-American sentiment. For their part, the city’s doctors and several local and national government officials claimed the Iraqi Ministry of Health had rigged the survey or skewed the data in an effort to kowtow to Washington.
“I’m sure either the work wasn’t precise or there was pressure to change the numbers,” said Dr. Chasib Ali, a high-level official in the Iraqi Health Ministry at the time the WHO-backed survey was conducted. “What I am sure about is that the data is not correct.” (The Iraqi Ministry of Health did not respond to requests for comment on Dr. Ali’s allegation.)
A few former WHO officials questioned whether the agency—caught between its mandates to serve the public health and to serve its member nations—could ever be a truly neutral party. “The WHO is a bureaucratic organization, and it has certain political influences upon it from its member states,” said Keith Baverstock, a former head of the radiation protection program at the WHO’s regional office for Europe.
The WHO declined to comment for this story. In 2013, however, the former WHO head of mission in Iraq, Jaffar Hussain, responded in The Lancet to critiques of the study. He said its data had been “extensively” reviewed by international experts and that its methodology was based on practices “renowned worldwide.”
As the medical debate continued to swirl, the mystery surrounding Fallujah’s children was deepened by yet another riddle: the potential reason for the spate of congenital defects. This question was always bound to be fraught, and what made it particularly so was the legacy of the United States’ use of depleted uranium during its two wars in Iraq. Depleted uranium is an extremely dense and mildly radioactive heavy metal that was first used during the 1991 Gulf War, when the US military sprayed approximately 1 million depleted uranium rounds across Iraq. While it serves mainly to reinforce tank armor and give bullets extra armor-piercing force, depleted uranium is perhaps better known for the harms some people fear it causes after battle: cancers, kidney diseases, neurological disorders, and birth defects.
The Pentagon has long said that depleted uranium does not pose serious health risks, yet concern about these harms ramped up almost as soon as the Gulf War ended. As doctors in the region began to report shocking increases in rates of birth defects and cancers, some Iraqi specialists attributed this rise to civilians’ exposure to depleted uranium. Others inside and outside the country pointed to additional factors, such as consanguinity (marriage between relatives, which is common in parts of Iraq) and improvements in diagnosing and tracking birth defects. The White House categorically dismissed the possibility of a connection between the diseases and its weaponry. Yet some of the Pentagon’s own research in the 1990s suggested links between depleted uranium and cancer and congenital disorders. In fact, prior to the Gulf War, a US Army report warned of “health risks to natives and combat veterans” from depleted uranium, including “potential radiological and toxicological effects.”
In the years that followed, the focus on depleted uranium intensified. Throughout the ’90s, the Iraqi government broadcast images of children with birth defects on national television and in major newspapers, blaming the US military’s use of depleted uranium for the disorders. “Look what their bombs have done to the children of Iraq,” read one newspaper article accompanied by a picture of a horrifically disfigured child. “They have turned Iraq’s children into target[s] of their [depleted uranium] weapons.” At the same time, as Gulf War veterans became sick with a collection of cancers and unexplained illnesses that came to be known as Gulf War syndrome, some in the United States began to point the finger at depleted uranium as well. Across the international stage, activists and experts organized symposia, demanded investigations, and called for a ban on the suspect metal.
Amid these calls, the scientific community conducted a number of studies to try to pin down just how toxic depleted uranium is. This remains an open and contested question. The Pentagon said its ongoing monitoring of Gulf War veterans exposed to depleted uranium has found “no adverse clinical effects” in the former troops and no birth defects in their children. The International Atomic Energy Agency also concluded the metal poses little threat in small amounts. But other studies continue to raise alarms, including some that found in vitro exposure to depleted uranium can cause genetic damage or mutations. (In these instances, the metal’s chemical toxicity, not its radioactivity, is believed to be the cause of harm.)
The competing studies contributed to the aura of conspiracy, and by the late 2000s, when Alani and other Iraqi doctors began to notice the birth defects, depleted uranium had become one of the most controversial substances on earth. Its notoriety was such that in Iraq and internationally, many were quick to view the reports of congenital disorders as evidence that the United States had used depleted uranium in Fallujah during the US invasion and its aftermath.
The challenge for those studying the issue was that the US military refused to disclose information about where and how much depleted uranium it had used during the war. It withheld these details even as some people in the Department of Defense became aware of the growing firestorm and warned of the dangers of failing to respond. As one Pentagon memo obtained by The Nation cautioned, “DoD has yet to acknowledge or publish any information regarding the quantity and locations of depleted uranium used during [Operation Iraqi Freedom]. In some ways this has been working against us.”
The Department of Defense did not respond to questions concerning why it had not publicly released this material. But critics say Washington’s silence only fueled the speculation—and, in the case of the Iraqi doctors looking to help their tiny patients, the desperation.
In 2013, Alani took her desperation all the way to the United States, to a conference organized by the Carter Center in Georgia. “On behalf of the women of Fallujah,” she begged, “I would like to call on the U.S. and U.K. governments to disclose information regarding all types of weapons used during the occupation and to take the measures necessary to protect the right to life and health of the local people if a pollution problem is indicated.”
The US and UK governments never responded to Alani. But over the next few years, the Pentagon provided answers of sorts to Wim Zwijnenburg, a project leader at the Dutch peace group Pax who has spent nearly a decade investigating the US military’s use of depleted uranium. In 2014 he joined with the New York–based Center for Constitutional Rights to file Freedom of Information Act requests with 10 US government agencies regarding this country’s use of the metal during the Iraq War. Most of the agencies did not respond—some because they said they did not have such records, others for no disclosed reason. But with the help of documents released by the Air Force in 2015, as well as documents shared by the National Security Archive, Zwijnenburg was able to begin piecing together a picture of where depleted uranium had been fired. Then, in June 2019, Zwijnenburg and the CCR received a batch of documents from the US Central Command that helped color in the picture.
The Centcom documents, which the CCR and Zwijnenburg shared exclusively with The Nation and which the Department of Defense authenticated, offer an essential, if not definitive, look at the range and extent of depleted uranium use during both of the wars in Iraq. They consist of some 200 pages of memos and reports along with maps showing where depleted uranium munitions were fired as well as the quantities. Still missing from the documents are 28 pages that were redacted or withheld on national security grounds. Moreover, the documents themselves acknowledge that it was “difficult to quantify exact DU use or exact DU locations.” But the revelations they contain are nonetheless significant, challenging long-held assumptions even as they raise new questions.
At the crux of the documents is the revelation that the United Stated deployed notably less depleted uranium in and around Fallujah than in other areas of the country. Specifically, the documents reveal that in March and April of 2003, the US military fired about 4,000 30-millimeter rounds, or 1.3 tons, of depleted uranium munitions in Fallujah—only a small fraction of the 69 tons the US military fired across Iraq that year. Most of that 1.3 tons was fired outside Fallujah’s residential areas. The documents also state that after April 2003, the US military did not use any depleted uranium in Iraq and that depleted uranium was not used during the fiercest battle in Fallujah in 2004. The documents also say that no depleted uranium was used in Fallujah during the 1991 Gulf War, when the US military fired 322 tons of it across Iraq.
For Zwijnenburg, who is an outspoken critic of the use of depleted uranium munitions, the documents offer a compelling case against the theory that the metal is to blame for the crisis of Fallujah’s children. Of note, he said, was that areas of Iraq that saw higher exposures did not have as many reported birth defects. “Considering the limited use, I find it difficult to link depleted uranium with the birth defects in Fallujah at the moment,” he said.
Douglas Brugge, the chair of the department of public health sciences at the University of Connecticut and an expert in environmental health, arrived at similar conclusions even as he cautioned that the documents could not reveal the full picture. (For that, he said, a case control study would be necessary.) “If you take the documents on face value, then specifically with regards to Fallujah, the amount of [depleted uranium] rounds that are actually fired and detonated seems modest to me,” he said.
“We get solely focused on depleted uranium because it’s associated with something that is so compelling and frightening,” he added, referring to the metal’s radioactivity, however weak. “But I would be surprised if it was the most widespread exposure and the most toxic exposure in a war like that.”
This new information, Zwijnenburg said, is not the end of the story but only the beginning of a much more complicated mystery. He said the absence of large amounts of depleted uranium does not absolve the United States or any other military actors from their possible roles in a health crisis in Fallujah. Instead, he said, the lack of transparency fueled fears about a specific substance, distracting from the need for a broader scientific inquiry for well over a decade.
“A larger focus on toxic remnants of war beyond munitions is needed to understand the environmental health risk,” Zwijnenburg said.
In interviews with The Nation, a slew of scientists, doctors, and anti-depleted-uranium activists concurred with Zwijnenburg, saying that the narrow focus on the metal has precluded an analysis of the overall public health and environmental effects of the conflicts in Fallujah and how they may be linked to birth defects. Alwani, the fetal medicine specialist who began photographing and recording the cases along with Alani, echoed this concern.
“I know every journalist concentrates on one point, which is the weapons,” Alwani said. “Weapons are not my issue. The problem is bigger than this.”
On the eve of the 2003 invasion, Iraq was already in the grip of a public health crisis. The military conflicts of the previous two decades had combined with the economic sanctions imposed by the UN Security Council to wreak havoc on the country’s environment and infrastructure. During the Iran-Iraq War of the 1980s, the Iraqi government manufactured and deployed chemical weapons, exposing military factory workers and some of its civilians to toxic gases. The 1991 aerial attacks by the US-led coalition destroyed the energy and sanitation systems. And the UN sanctions, imposed in 1990, hampered the reconstruction of essential electrical plants and sewage treatment facilities. The ban on importing chlorine rendered water purification next to impossible.
The sanctions also devastated the country’s health care system, which was regarded as among the best in the region. The system’s budget was cut by 90 percent during the 1990s as the embargo crippled the economy. Although medicine was ostensibly exempt from the ban, expired or untested medicines flooded the black market. As food grew scarce, the per capita caloric intake for Iraqis plummeted to as low as 1,093 per day in 1995, according to a brief by UNICEF and the WHO, leading the health agency to observe in a 1996 report, “The vast majority of the country’s population has been on a semi-starvation diet for years.”
“The quality of health care in Iraq, due to the six-week 1991 war and the subsequent sanctions imposed on the country, has been literally put back by at least 50 years,” the WHO concluded.
Omar Dewachi, an Iraqi doctor and medical anthropologist who has been documenting the health impacts of conflict in the country for decades, witnessed the effects of the sanctions while he was working at a public hospital in Baghdad in 1997. “We had much higher cases of malnutrition, which had been eradicated in the ’60s,” said Dewachi, whose book Ungovernable Life traces the history of the health care system in Iraq.
The government’s food rationing system, imposed in response to the sanctions, staved off a potential famine but left people deficient in several vitamins and minerals, including nutrients essential to fetal development. According to the 1996 WHO report, the availability of folate—which helps prevent serious congenital disorders known as neural tube defects—decreased more than 77 percent. The ration diet more than halved the availability of zinc and riboflavin, deficiencies of which are linked to some birth defects, as well as thiamine, a deficiency of which can increase the risk of stillbirth. By 2003, UNICEF said, nearly 60 percent of the Iraqi population was fully dependent on food rations, meaning that these nutritional deficiencies affected more than half of the population. The Ministry of Health recorded a national rise in congenital heart disease, one of the most common types of birth defects, between 1991 and 1998.
“Nutritional factors are known to cause congenital anomalies and defects, and that has been a very understudied pathway for birth defects in Iraq,” said Dewachi.
In Fallujah the US invasion and its aftermath severely exacerbated these underlying health and environmental problems. In 2004 the city was the site of the bloodiest battles of the US war in Iraq. In November and December, nine US Army and Marine battalions laid waste to Fallujah, destroying or damaging tens of thousands of homes, multiple water treatment facilities and power plants, and the city’s sanitation system. The battle killed thousands of Iraqis and 82 Americans. Raw sewage flooded the streets. Dogs mangled bodies that were strewn across the city. US troops deployed white phosphorus, a chemical weapon capable of burning skin and muscle down to the bone. It was a battle the US forces fought with a spirit of vengeance because, as Defense Secretary Donald Rumsfeld and other top US leaders saw it, “Fallujah had become a symbol of resistance” to the US occupation of Iraq.
Liqaa Wardi, a former parliament member from Fallujah, recalled how her husband, an engineer, was flown into the city on a military helicopter and tasked with surveying the damage in the siege’s aftermath. “He told me the city was flooded by water, bodies were everywhere, and there were a lot of obstacles and challenges to reconstruction,” she said. Over the ensuing months, displaced residents—including Alani and her family—returned to Fallujah and set about rebuilding their city. But the precarious security situation at the time made it impossible for members of the environmental ministry or the UN Environment Programme (UNEP) to study the damage firsthand.
A slew of factories, chemical warehouses, and military industrial buildings in and around Fallujah posed hazardous risks to nearby residents. The UNEP highlighted many of these sites in three reports published between 2003 and 2005. One of the country’s largest chemical warehouses, in Khan Dhari, about 20 miles from Fallujah near Abu Ghraib, was ransacked in the aftermath of the US invasion. (The report does not identify which parties looted and set aflame parts of the complex.) Hundreds of tons of hazardous materials at these warehouses were spilled, burned, or stolen, including the highly toxic chemicals tetraethyl lead, furfural, methyl ethyl ketone, and sodium hydroxide. Other sites were not destroyed but nevertheless posed pollution risks. A military manufacturing site near Fallujah contained cyanide and heavy metals, and a cement plant spewed pollution, possibly including arsenic and dioxin (a chemical in Agent Orange), both of which have been linked to birth defects. (The Department of Defense did not respond to questions about these reports of widespread environmental contamination.)
All these chemicals potentially mixed with pollutants left from earlier conflicts. In 1991 and 1998, for example, the US bombed a chemical weapons complex and pesticide production factories in the area—collectively known as Fallujah I, II, and III—polluting the soil at the site. In the 1980s, residents of Fallujah may have been exposed to serious toxins by serving in the Iraqi Army or working at military factories where health and safety measures were scant.
Such pollution was not unique to Fallujah. In 2005 the UN estimated that Iraq was littered with several thousand contaminated sites. Five years later, a Times of London investigation revealed that the US military had generated over 10 million pounds of toxic waste and that it was abandoning hazardous material in dump sites along main roads. The same year, an Iraqi government study undertaken by the environment, health, and sciences ministries discovered more than 40 locations across Iraq, including at least one site in Fallujah, that were contaminated with radiation or dioxin. Hassan Partow, the program manager of the UNEP’s crisis management branch, was part of the environmental assessment team in the immediate aftermath of the invasion. “Iraq’s environmental contamination is one of the more serious cases of conflict pollution that UNEP has investigated,” he told The Nation, pointing to “chronic, multiple, and widespread causes of pollution.”
Yet even amid the nationwide environmental crisis, Fallujah’s toxic legacy stood out. “Fallujah was the city in Iraq with the highest contamination,” Abdul Kareem Al-Samari, the Iraqi minister of technology and science from 2010 to 2014, told The Nation. Alarmed by the reports of rising rates of birth defects and cancer in Fallujah, he said he sought to establish local centers to study diseases and contamination during his time as minister, but the initiatives were never completed. Health-related funding, he said, always seemed to disappear amid corruption or was diverted to the military budget.
The Iraqi government did not respond to questions about why the research centers aimed at studying birth defects and cancers in Fallujah were never completed. However, Jassim Abdulaziz Humadi Alflahy, Iraq’s deputy minister of health and environment, said in an interview that, in general, years of conflict, including the 2014-2017 war against the Islamic State, have compelled the government to siphon resources away from social programs.
Alflahy also said the alleged increase in birth defects in Fallujah could be linked to this broader environmental crisis, although he was careful not to draw a causal conclusion. He, like other officials, said improvements in the diagnostic and registration system for congenital abnormalities explained part of the reported rise. “But sometimes we might—and we insist on ‘might’—relate it to the pollution: air pollution, water pollution, soil pollution with heavy metals, radiation, chemical pollution, because as I said, we are facing decades of war,” he added.
Dewachi explained that the challenge of studying birth defects in Fallujah and across Iraq comes down to this fact: The disorders cannot be easily linked to a single cause. “You are dealing with a complex ecosystem of toxicity and interactions,” he said. “I think there is a kind of obsession of finding a magic bullet to explain the birth defects in Iraq…. People have been trying to attribute it to a specific weapon like depleted uranium—everyone wants depleted uranium to be the culprit—and it’s the search for the culprit that I feel has been missing the forest for the trees. We’re missing the bigger picture of how, over decades, there has been a systematic production of toxicity in the everyday life of Iraqis.”
For Dewachi and others, this bigger picture doesn’t preclude the question of culpability. But it does, at least in the case of Fallujah, force one to reconsider the search for a single toxic substance and instead grapple with the possibility that 21st century urban warfare, in and of itself, might unleash intergenerational damage that we are only beginning to understand.
“This is a part of the unresolved mystery of these birth defects,” he said. “It makes us ask: How do we move forward? How can you really think about accountability for these kinds of questions?”
Seventeen years after the United States invaded their country, Alani and her colleagues still don’t know exactly how or even if the conflict is related to the birth defects she says she witnesses in the hospital daily. On another hot September morning last year, she sat in her small, dimly lit office before her rounds in the maternity ward. She was exasperated by the morning traffic, and she seemed tired. Over the years, she has authored or coauthored more than a dozen studies, challenged the WHO, and traveled to the United States to appeal to the former president Jimmy Carter for information about the US-led battles in her city. She has survived air strikes and two foreign military occupations. And her family members have lost children to the very birth defects that she has sought to treat.
She pulled out a copy of a letter that, she said, the hospital sends to the Health Ministry in Baghdad each month to request new equipment, including a gamma blood irradiator, a Cobas E 411 analyzer for in vitro diagnostic tests, and a newborn screening system to identify genetic and metabolic disorders. So far, she said, the equipment hasn’t arrived, but she intends to continue requesting it. “We are looking to find solutions for these families,” she said.
As Alani prepared to see her patients, Alwani entered the office. They recalled when they began to record cases about a decade ago, with Alwani taking photographs with a camera because they didn’t have smartphones yet. Alwani said she never intended for the images to be used as political symbols. “I don’t like to transmit the tragedy of the people,” she said. “I was thinking to solve the problem, not to reproduce the problem.” Over time, however, the images of Fallujah’s dead and deformed babies transformed into emblems of the war’s long-lasting and gruesome consequences. Plastered on poster boards and anti-war websites, the photos became symbols of the irreversible and intergenerational impacts of a war that most Americans now call a mistake. But the city’s children, Alani and Alwani said, are still suffering with little fanfare.
A few weeks later, Alani published another case study in the Asian Journal of Case Reports in Medicine and Health. In the peer-reviewed paper, she analyzed twins born in the Fallujah hospital with two different severe disorders. She wrote that the second child, a boy, was dead when he emerged with his blue intestines heaving out of his abdomen. The first infant entered the world alive. But the child wouldn’t survive long, Alani knew, not with the two tiny legs fused together. Both children reminded her of other deformations she’d seen and recorded in her hospital, but never had she seen the two rare syndromes in the same pregnancy.
Alani concluded her case study with a dry observation. “The high prevalence of birth defects in Fallujah is impairing the population’s health and [its] capacity to care for the surviving children,” she wrote. She added that the problems were exacerbated by limited prenatal care, lack of support for families with birth defects, and “the absence of clear serious future plans for improvement of the health system or taking serious measures to clean the post wars contaminated environment.”
What she didn’t write about was how the father of the twins became hysterical after the delivery and refused to let her perform X-rays or ultrasounds on them. He simply took the first child out of the hospital to die at home, leaving Alani to write down the limited information she was able to collect, hoping that the record, even if incomplete, would someday benefit her patients.N